Personal patient story – Eating is not a luxury and food is much more than nutrition
Video URL: https://www.youtube.com/watch?v=wiqkT8F-br4
Let’s talk about food for a minute.
Can you imagine not eating for a week? A month? How about a Year? Five Years?
Can you imagine cooking for your family without being able to join in the meal?
Without even tasting to decide if it is salty enough?
Can you imagine doing it week in week out, month after month and year after year?
Can you imagine giving in to temptation every now and then, having just a bite or two and then regretting it immediately while you suffer unbearable pain that lasts for hours and sometimes even for days?
Now imagine you’re going through all that while carrying a backpack in which sits an external feeding set to which you are connected for 20 hours a day…
This is how I live. I haven’t eaten a full meal since 2009.
My name is Orna Resisi, I am 57 years old and I live in Tel Aviv, Israel. I am married and a mother of 3 wonderful children. I am a senior computer software engineer and I work full time at the Center for Educational Technology where we develop technological platforms and content for the educational system. I love extreme activities such as paragliding, rafting, hiking and diving. I love babies and children. I read a lot, mainly about relationships and family sagas. I have been a type 1 diabetic for the past 30 years.
I want to tell you a little about my life these last 10 years.
MY MEDICAL STORY
I was diagnosed with Insulin Dependent Diabetes (also known as IDDM or type 1) in 1986. From the start my Diabetes was very hard to manage. Despite constant daily monitoring up to 15 times a day, (and) keeping records of food and insulin intake versus sugar levels and despite close supervision by leading medical professionals – my blood glucose levels have never stabilized.
Whilst normal levels range between 70 – 99, my levels peak at 30 – 450. Sometimes I go through several hypoglycemia (very low glucose levels) and hyperglycemia (very high glucose levels) events a day knowing that I am constantly on the verge of unconsciousness as a result of the lows and that each high contributes to unimaginable accumulative bodily damage part of which I am already experiencing, part of which I will have to deal with in the not so far future.
High glucose levels damage the blood supply to nerves (diabetic neuropathy) and as a result I suffer neck, shoulder, back and leg pain which have been quite disabling over the years. There were times I could not walk because of the pain. I also suffer from migraines which may be, or may not be a complication of diabetes.
During the last 10 years I have seen dozens of medical experts. They range in their field of expertise. Some were Gastroenterologists, others were Endocrinologists, Neurologists and Pain Management specialists.
I have gone from one expert to the other seeking help and relief, but despite occasional glimpses of hope I have constantly been let down. Not because they didn’t want to help me, but because they couldn’t. Science, or medicine, or the health service aren’t there yet. This is why I’m here today.
With all their accumulated knowledge and experience they have never seen a patient in my condition and most of them were quite surprised I was alive.
I was forced to accept the fact that at best, each specialist could address one specific aspect of my complex condition. It was always just one aspect. Either the nutritional components, the pain management, the gastrointestinal aspects, the orthopedic aspect of back and limbs, the migraines, the side effects of the medication… but none of them could fully grasp my condition in its’ entirety.
None of them could see me as a whole. I am bringing this up today because I want you to get a glimpse of me. This is me. This is my life.
Put yourself in my shoes. Could you face a future that does not promise any change?
But for today, this is all in the background as I am here to talk about food.
In 2005 I was diagnosed with gastroparesis, a disorder that slows or stops the movement of food from the stomach to the small intestine. This makes you feel bloated and nauseated following every meal.
In 2006 I developed a severe case of Ischemic Colitis. I was rushed to the hospital in critical condition and I was hospitalized for 3 months living on intravenous nutrition so that my digestive system could rest and recover. Because the nutritional solutions are highly concentrated and thick, they must be administered through catheters that are placed in large central veins in the neck, chest, or groin.
While the central line was being put in my lung was punctured and I spent the next few days in ICU. I was treated with morphine because of the severe pain I suffered.
This hospitalization was just the beginning of my journey into the exciting world of Gastro intestinal problems. I spent the 3 years that followed in and out of hospitals, for periods extending from days to weeks. My constant problem was very severe stomach aches which at times were so severe that I could not eat for days.
In the beginning of 2009 I was diagnosed with CIPO (Chronic Intestinal Pseudo Obstruction) secondary to diabetic neuropathy. This is a condition caused by severe impairment in the ability of the intestines to push food through, resulting in pain which inhibits the desire to eat. It feels like the nerves send a signal of extreme pain whenever they detect food.
Things got worse and by the summer of 2009 I could no longer eat at all. I lost weight and with it I began losing my vitality. My dietician put me on an oral diet of Peptamen, a canned formula intended for people who cannot digest.
I was instructed to consume at least 1500 kcal a day but I only managed to take in 500 kcal as even swallowing the formula caused considerable pain. I deteriorated rapidly, lost 15 additional kilos in 6 months and became so weak that I was completely dysfunctional. I felt as if I were 100 years old, and even walking across a room was too big an effort.
I was in a state of extreme malnutrition by the time I was referred to the Nutrition unit in Rabin Medical Center, headed by Prof. Pierre Zinger.
At his instruction a Hickman catheter was implanted into my chest and I was put on Total Parenteral Nutrition (TPN), a feeding method aimed to prevent and/or treat malnutrition. TPN provides essential nutrients which the patient receives intravenously, in order to bypass the dysfunctional or absent digestive system. An infusion pump controls the rate at which the TPN solution is given, so that the concentrated food does not overload other digestive organs. TPN can be administered at home, and after my husband and I were taught how to administer it I was released home. This was in the winter of 2009, and it was a turning point as it was the TPN and Prof. Zinger’s team that brought me back to life.
I was connected to the TPN for 20 hours a day – for 5 years. Each night I would sterilize myself, create a sterile field and connect to a 2 Liter bag of nutrition. I would put it in my backpack, together with the pump, and it would feed me in my sleep. In the morning I would shoulder my pack and go to work.
Every time I moved from my seat I would have to take my backpack with me. I would return home from work around 18:00, and an hour or two later the feeding process would end and I would once again sterilize and disconnect myself. Every evening I had around 3 hours in which I was free to move around without my extra baggage. Then I would shower and the whole ordeal would start over again.
During those five years, every week a delivery van from TEVA Pharmaceuticals would bring me my nutrition and required supplies for the week. Six big boxes full of supplies – sterile kits for connecting to the TPN, sterile kits for disconnecting, filters, syringes, dressings and such. Our house began to look like a hospital and we had to empty a shelf in the refrigerator just for the formulas.
If I wanted to change my plans, go out on the delivery day or such, I would have to coordinate this with the representative of the pharmaceutical company, and they became a part of my weekly schedule, gradually getting to know where my mother lived, and where my sister lived as they became alternative drop off points for supplies.
Every month I would meet with the Prof Zinger’s Nutrition Team to check my progress, and every time changes to the basic formula were made based on the results of my blood tests.
Some of the complications of TPN which I experienced were TPN-induced liver damage, which in my case was detected very early and was therefore thankfully reversible.
I also experienced further serious complications such as a clot (thrombosis) in central access veins, and frequent infections in the central-vein access lines. These infections can quickly become life threatening due to proximity to the heart. During one of the years I was on TPN I was hospitalized twelve times. As a result of the infections and the clotting the catheters had to be replaced 9 times in 5 years. Each replacement involved another operation.
At one time I had 2 central line catheters at once, one for nutrition and the other for anti-biotics, intended to fight off the infection so that the main line could be kept alive… During those years I became utterly dependent on TPN for my life. Without the superb supervision of Prof. Pierre Zinger and his team of experts from Rabin Medical Center in Israel to whom I am extremely thankful, I would not be alive today.
Everything looked like the TPN was here to stay, a part of my life forever.
For 5 years I completely refrained from eating. However the pain was still there, ever present. Neuropathic pain is a complex, chronic pain state in which the nerve fibers themselves may be damaged, dysfunctional, or injured. These damaged nerve fibers send incorrect signals to the pain center in the brain. Living with chronic pain is very difficult and depressing and takes a heavy toll on a person’s wellbeing and mental state. It is also a heavy load for the family.
I was treated with medications, narcotics and nerve blocks. In 2013, a stimulating device was surgically implanted in my spine and connected to several nerve roots in an attempt to alleviate some of the pain. This procedure had partial success.
Unexpected change of events
In 2014, following 12 long weeks of constipation, I was given an experimental medication to encourage my colon to work. A week later my colon perforated and its contents spilled over into my abdominal cavity. I was rushed into an emergency surgery which lasted 8 hours and saved my life.
When I woke up a few days later in ICU, I no longer had a colon. It was completely removed, and in its place two stomas were created – a feeding stoma in the jejunum and an ileostomy through which digestive contents now leave the body. The drainage is collected into an external pouch that sticks to the skin around the stoma.
At this stage the TPN was replaced by enteral feeding of ALITRAQ formula through the jejunum. Enteral feeding is an improvement in terms of the reduced risk of life threatening complications associated with TPN. It is also a much simpler daily routine as it does not require sterile handling. Currently I require only 10 hours of daily infusion as opposed to the 20 hours of TPN.
On the other hand living with an external pouch can be quite depressing, annoying, and very embarrassing at times, and it takes time getting used to. Issues such as gas, increased odor, thickened or thinned stool, incomplete digestion, skin rashes, leaks, spills and overflows from the pouch have to be regularly dealt with, and can cause embarrassment, unease and increased self-awareness.
After the removal of my colon in 2014 the surgeons expected that within a short time I would be able to eat normally but as it turned out- I couldn’t. My stomach does not respond well to oral nutrition, and recurrent attempts of eating actual food still result in severe abdominal pain, nausea and bloating. Unfortunately the Gastroparesis and the Chronic Intestinal Pseudo Obstruction still exist in the remaining parts of my digestive system.
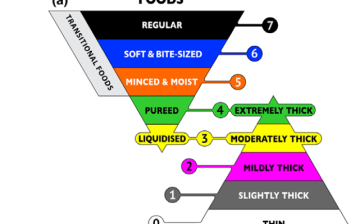
My oral diet is limited to minuscule amounts. I can eat a rice cake or two, plain yogurt or some cheese and an occasional hardboiled egg, but not all at once. When I can’t bear it any more I usually eat a slice of bread or a few spoonful of rice, sometimes a cookie. They are the most comforting and cause the least pain but they do of course raise my glucose levels. I love ice cream, and sometimes can’t resist it, but I always end up regretting it.
My body cannot tolerate any amount of fruit or vegetables or anything containing fibers. Meat, poultry and fish as well as any fatty foods and anything that is fried cause pain and nausea. I am also limited to drinking very small quantities, not more than a few gulps. If I go over the limit I suffer for hours afterwards.
Emotional Aspects – Food is so much more than nutrition!!!
During my five years on TPN I was constantly hungry, and the mental and physical craving for food is something which the doctors failed to understand, and which nobody could help me deal with. Sometimes I felt I was going crazy with hunger.
Not being able to eat like any other person is socially alienating and very depressing, and the truth is that being able to eat a very limited diet is not much easier than eating nothing at all. I have a dream that one day I will be able to eat like any normal person, with no painful consequences. Juicy hamburgers are the main stars in my fantasies.
(Just as I was writing this there was an item in one of the news magazine programs on TV about a startup company that is developing a system in which a person could taste and smell food and get the feeling as if he or she were actually eating using Virtual Reality. Maybe that is where my dream will come true)
At work, most of the work-related social activities as well as part of the professional decisions take place over lunch, which I avoid going to and therefore am left out of.
At home, family meal times are very hard. I cook for my family, and then sit at the table watching everyone else eat, without being able to participate in the meal. I don’t allow myself to be absent from those meals because I don’t want to lose out on precious quality time with my family.
When I was on TPN I also felt ‘left out’ of almost all of the fun aspects of the world:
Meals, restaurants, cafes, were all out of bounds for me. But so were daily recreational activities such as the beach or the pool, spa and water sports, a Jacuzzi or even a bath – I couldn’t do any of these as contaminating the catheter was too big a risk.
Going on holiday (once I felt up to it, and once Prof. Zinger allowed it) was very difficult logistically and limited to a week at most because that was the longest period of time that I could go without my custom tailored TPN which required refrigeration and was only stable for a week. When I did go away, I would need to carry 15 Kgs of formula plus all the equipment needed for connecting and disconnecting in a sterilized environment…
Now that I am off TPN I no longer need to worry about infections, but who wants to go swimming with an external drainage pouch connected to his belly…
Logistical Aspects
Although the change from TPN to enteral nutrition was actually good news, at the time it felt like a blow. TPN had its many disadvantages, but at least all the equipment I needed was regularly delivered to me. This changed when I was put on enteral nutrition.
While still weak from the major surgery I had undergone, I discovered that it was up to me to get hold of the pump, the feeding bags and nutritional formula, as well as all the stoma equipment I needed by the time I was to be discharged.
The pumps available through the health services are big and clumsy and seriously restrict daily life. They are designed for bedridden people, but I want to be active. As a result, I had to purchase an alternative, more user friendly, feeding pump and the matching formula privately. The feeding bags available through the health services are of poor quality and regularly leak. To this day a year and a half after beginning the search, I still struggle finding a feeding bag that won’t leak or fall apart.
Knowledge and information
Right after my surgery I was told that my bowels would respond to a gradual introduction of regular foods. I was instructed to eat whatever I wanted and was encouraged and even pushed to do so despite the pain. The surgeons tried to convince me that the pain I was experiencing was not real, that it was all just in my head.
A year passed before a junior dietician I met completely by chance asked me why I was trying to eat foods such as fruits vegetables. She was stunned to realize I had not been informed that without a colon the body finds it very hard to digest any kind of fiber.
Economical Aspects
- COST OF ARTIFICIAL NUTRITION
| Product | Who pays | Price per Day | Price per Month |
| Peptamen | Patient | 45 € / Day | 1350 € |
| TPN | Health Services | 230 € / Day | 6900 € |
| AlitraQ | 80% Health Services | 60 € / Day | 1800 € |
- SENSORS AND CGM
Continuous glucose monitoring (CGM) via SENSORS is the most efficient method available today to track blood sugar levels and avoid life threatening situations caused by sudden uncontrolled changes. Yet CGM is not included in the health basket for adults.
Despite life threatening hypos I experienced, I was not found eligible for financing and privately I could not afford it. Needless to say this has had a huge impact on my health and wellbeing, as well as on future complications I will no doubt have to face.
Adding CGM to the health basket would make it available to all unstable diabetics thus helping them maintain a more balanced life which in turn would save the health services greater expenses in the future.
Summary
I have lived in agonizing, chronic pain for many years. In spite of that, I have done my very best even at darkest of times, and have managed to raise a family, work full time and volunteer for causes I believe in. I have lead a normal life in abnormal circumstances.
I am not a hero. I have been blessed with a very strong mental ability and an extremely supportive family who do their very best to help me carry the load.
I know that I am very lucky to have been able to come here today to share my story with you. I feel a heavy weight of responsibility to be a voice for all those with rare and unknown conditions who are not able to speak out.
My appeal to policymakers, is:
- To raise the awareness to the dangers of malnutrition and the existing techniques that can deal with it.
- To direct the needed funds to the scientific and medical research, for the development of medications, modern surgical techniques and neurological interventions.
- To develop a one stop multidisciplinary service by creating holistic clinics with holistic medical teams who will diagnose, treat and support patients with complex needs.
- To encourage sharing of information and expertise of these holistic centers so that patients can benefit from experience gained in other parts of the world.
- To include CGM in the provided health services so that all diabetics who need it can have access to it.
- To broaden the criteria that determine which diseases are eligible for financing of medical nutrition.

Personal patient story - Eating is not a luxury and food is much more than nutrition
105.53 KB
Download