The National Program for Quality Indicators in Community Healthcare in Israel
In 1995, Israel enacted the National Health Insurance (NHI) law providing a standardized basket of medical services to all residents by the four health plans, and stating that “healthcare services included in the basket of medical services will be offered based on medical considerations, with reasonable quality, in a reasonable timeframe, and at a reasonable distance from the place of residence of the insured person”.
In light of the above, the need for the assessment of the quality of medical care in Israel led to the establishment in 2004 of the National Program for Quality Indicators in Community Healthcare in Israel, funded by The Israel National Institute for Health Policy Research.
The Program is led by an academic directorate and full cooperation of the health plans with Program’s directorate in setting quality indicators, assessing the indicators on a regular basis, and publishing them are noteworthy cornerstones of the Program’s success.
The Program aspires to provide the public and policymakers with information regarding the quality of healthcare provided by the health plans in community setting in order to improve medical care offered to Israeli residents.
Data and Population
The Program directorate receives anonymous aggregated data provided by Israel’s four health plans, based on information from patient’s electronic medical records.
As under the NHI law mentioned above, all Israeli citizens enjoy universal health coverage and therefore the National Program for Quality Indicators in Community Healthcare’s data practically includes the entire Israeli population.
Collecting and reporting data for the entire insured population in Israel enables the assessment and monitoring of the quality of healthcare for smaller sub-groups, identified by age, gender, and socio-economic status. Socio-economic status is determined based on exemption from co-payments for health services. In 2015 that the exempt population was 11.5% of the total population. However, among persons 65 years and above, this rate reaches 30%. Exemption is given by a number of criteria, including allowances from the National Insurance Institute such as handicap allowance.
Body weight documentation and detection of underweight and weight loss in the elderly are important steps for preventing morbidity and mortality among this population. Documenting body weight is essential to preventative care, as by providing information on patients’ weight status compared to the recommended healthy weight status, nutritional needs, medication dosing, and specific health problems may be implied [2].
Underweight in the elderly has been associated with excess mortality, as compared to those with a normal weight [3]. Instability in elderly weight has also been associated with all-cause mortality [4], and monitoring elderly weight changes over time assists in understanding the quality of elderly health. Moreover, dynamic body weight measures (i.e. weight changes), compared to static body weight measures (e.g. body mass index), better predicts mortality among the elderly [4]. Weight loss has been associated with elderly health conditions, such as frailty. Frailty is associated with increase odds for falls, hospitalizations, longer hospital stays, delayed surgery recovery, disability, and death [5-7].
Underweight in the elderly is defined as follows
Denominator
Number of residents aged 65 or older during the measurement year with body weight and height documentation (documented body weight during the measurement year and at least one height documentation after 65 years of age).
Numerator
Number of residents (out of the denominator) with most recent documented BMI< 23 Kg/m2.
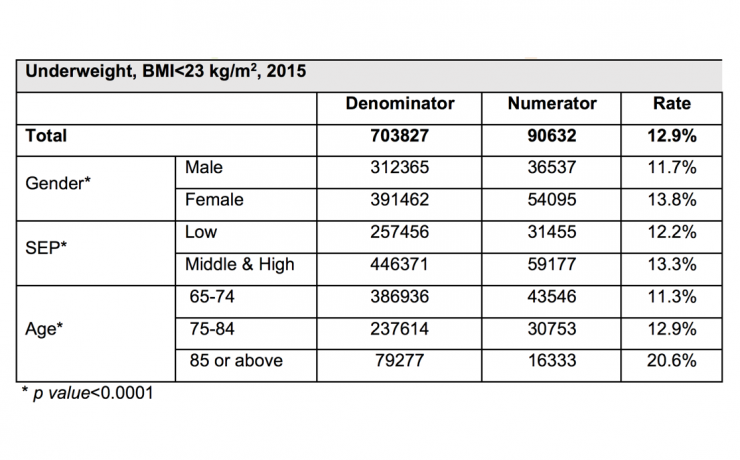
Table 1: Underweight in the elderly: rates by gender, SEP, and age groups, 2015.
The rate of underweight (BMI<23 kg/m2) among the elderly Israeli population in 2015 was 12.9%. The prevalence of underweight was found to be higher in female compared to male (13.8% vs 11.7%, respectively, p<0.0001, table 1). This gender-difference was mostly pronounced within the younger age group (65-74 years-old), with an absolute difference of nearly 3% in the prevalence of underweight between female and male; while less than 1% difference between genders was found in the older age groups (0.4% in 75-84 years-olds, and 0.8% in 85 years-old or older, data not shown).
Individuals of low SEP were less likely to be classified as underweight, compared to those of middle-high SEP (12.2% vs 13.3%, respectively, p<0.0001, table 1). The prevalence of underweight significantly increased with increasing age (from 11.3% among those 65-74 years-old, and up to 20.6% among those aged 85 or older, p< 0.0001, table 1).
Underweight and significant weight-loss were more frequent among females than among males, and substantially increased with increasing age.
References
- Cohen R, Rabin C. HMO Membership 2015. Periodic Survey 271 edition. Jerusalem, Israel: National Insurance Institute- Research and Planning; 2016. https://www.btl.gov.il/Publications/survey/Documents/seker_280.pdf
- Evans L, Best C: Accurate assessment of patient weight. Nursing Times 2014, 110:12-14.
- Winter JE, MacInnis RJ, Wattanapenpaiboon N, Nowson CA. BMI and all-cause mortality in odler adults: a meta-analysis. Am J Clin Nutr. 2014; 99(4): 875-90.
- Somes GW, Kritchevsky SB, Shorr RI, Pahor M, Applegate WB: Body Mass Index, Weight Change, and Death in Older Adults The Systolic Hypertension in the Elderly Program. American Journal of Epidemiology 2002, 156:132-138.
- Alibhai SMH, Greenwood C, Payette H: An approach to the management of unintentional weight loss in elderly people. CMAJ: Canadian Medical Association Journal 2005, 172:773-780.
- Buckinx F, Rolland Y, Reginster J-Y, Ricour C, Petermans J, Bruyère O: Burden of frailty in the elderly population: perspectives for a public health challenge. Archives of Public Health 2015, 73.
- Pandya N, Rokusek C: Undernutrition and weight loss in the elderly. Nova Southeastern University.