
The International Working Group for Patients’ Right to Nutritional Care position paper was published in Clinical Nutrition, the Official Journal of ESPEN (The European Society for Clinical Nutrition and Metabolism) on the 20th of May 2021.

The position paper presents nutritional care as a human right, intrinsically linked to the right to food and the right to health. All people should have access to food and evidence-based medical nutrition therapy including artificial nutrition and hydration. In this regard, the hospitalized malnourished ill should mandatorily have access to screening, diagnosis, nutritional assessment, with optimal and timely nutritional therapy in order to overcome malnutrition-associated morbidity and mortality, while reducing the rates of disease-related malnutrition.
Application of the human rights-based approach to the field of clinical nutrition will contribute to the construction of a moral, political and legal focus to the concept of nutritional care. Moreover, it will be the cornerstone to the rationale of political and legal instruments in the field of clinical nutrition.
“Health and human rights are complementary approaches for defining and advancing human well-being. The goal of linking health and human rights is to contribute to advancing human well-being beyond what could be achieved through an isolated health or human rights-based approach (HRBA)”
Despite the evident rapport, clinical nutrition has never been examined under such a perspective. This is why an international working group was launched in 2020 to explore how the Human Rights-Based Approach (HRBA) can contribute to the challenges faced by the practice of clinical nutrition in increasingly demanding health care systems. The working group is composed of experts in clinical nutrition and representatives of ASPEN, ESPEN, FELANPE, PENSA, WASPEN and SASPEN. Therefore, the aim of this position paper is to provide the link between clinical nutrition and human rights, in an attempt to characterize nutritional care as a human right, and thus highlight the need for early diagnosis and treatment of DRM as a holistic process of patient care.
Video URL: https://www.youtube.com/watch?v=sUDw8ziwuOc
The HRBA is a conceptual framework that can be applied to clinical nutrition.
“The Human Rights-Based Approach is normatively based on international human rights standards and operationally directed to promoting and protecting human rights”
Applied to the healthcare context, this approach focuses “on the underlying social determinants of health and on emphasizing the principles of accountability, meaningful participation, transparency, equality, and non-discrimination” (1)
Clinical nutrition has not yet been explored in the context of HRBA. Until now, it has been limited to promoting and claiming the right to food in the clinical context. (2,3)
But why is the right to food neglected in the clinical field?
The hypothesis is that disease-related malnutrition (DRM) does not fall within the scope of the concept or normative content of the right to food. Moreover, the right to food is within the scope of community malnutrition, a distinct form of malnutrition, the origin of which lies in food insecurity. There are different pathways of community malnutrition and DRM. It must be noted that according to the particularities of each form of malnutrition, a different approach is needed. (See Figure 1 of the article)
The working group advocates that it is necessary to recognize nutritional care as a human right
The definition of nutritional care as a human right
The foundation of the right to nutritional care
- Human dignity
- Ethical principles
The duty-bearers
- The state, policymakers, institutional managers, and caregivers
The content or scope
- The human right to benefit from the whole process of nutritional care. This means that the patient has the right to beneficiate from the right to be screened and diagnosed for disease-related malnutrition, to receive regular hospital diet, therapeutic diet (i.e., food modification and supplements), and evidence-based medical nutrition therapy (i.e., AANH) administrated by an interdisciplinary team of experts, and the government has the duty to guarantee it. (4)
Fulfillment of the right to nutritional care requires the following mandatory actions
Nutrition screening at hospital admission and during the first clinical contact in primary care
Diagnosis and assessment of malnutrition in all at-risk patients
Provision of a regularly monitored nutrition care plan, by:
- Maintaining a regular oral diet, or, if precluded by the patients’ clinical condition
- Implementing evidence-based medical nutrition therapy/artificially administered nutrition and hydration (AANH).
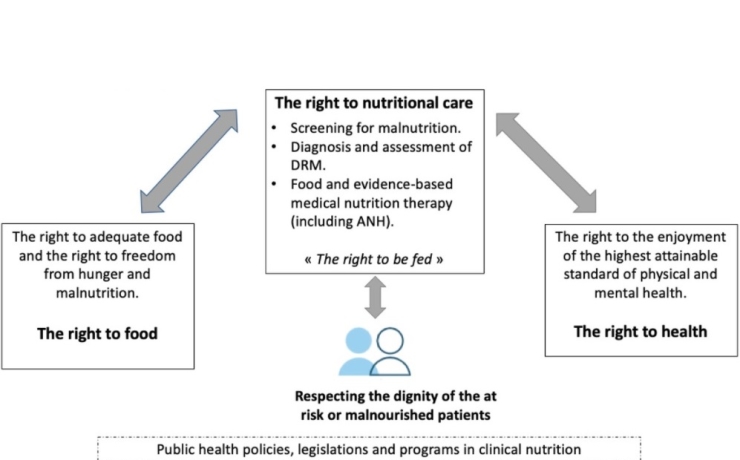
Nutritional care is at the intersection of the right to food and the right to health, therefore creating opportunities for the implementation of rights-based legislations, policies, and programs for its realization. DRM, Disease-related malnutrition; AANH, Artificially Admininstered Nutrition and Hydration
Finally, the realization of the right to nutritional care must be a goal of state policies and programs regardless of their economic, social, cultural, religious, or political background. To achieve this, the international working group recommends the following 10 principles:
- Public health policy must make the fulfillment of the right to nutritional care a fundamental axis in the fight against DRM;
- Clinical nutrition must be integrated into public health policy based on human rights, equity, and economic values;
- Clinical nutrition education and research is a fundamental axis of the respect and the fulfillment of the right to nutritional care;
- Ethical principles and values in clinical nutrition including justice and equity in nutritional care access are the basis for the right to nutritional care;
- Clinicians, researchers, and policymakers should work together to translate evidence-based medical nutrition therapy into policy;
- To be effectively implemented, public health policy on clinical nutrition should consider all patients at nutritional risk, including childbearing women and children, as the target population;
- Public health policy should consider nutritional care as part of the holistic approach for the patient, which aims to prevent and treat DRM and improve clinical outcomes;
- Nutritional care requires an institutional culture that follows ethical principles and values, and an interdisciplinary approach;
- All nutritional care must include an after-hospital discharge plan, involving patients and caregivers, and be subject to an annual audit;
- Patient empowerment is a key enabler to necessary action to optimize nutritional care.






