Malnutrition can occur at any age. However, upon closer analysis, it is primarily a problem for seniors over the age of 65. Regular nutritional screenings are crucial for early detection, as well as rapid and targeted nutritional interventions; and can prevent a great deal of suffering for those affected. Replenishing nutrient reserves can increase the physical and cognitive functions of patients and thus have a decisive influence on their quality of life. This is the conclusion of an interdisciplinary panel of leading Austrian nutritional experts. On the initiative supported by Nutricia Milupa, the panel discussed this highly relevant topic in the context of a scientific roundtable and subsequently drafted a corresponding recommendation paper, which was published as a supplement to the “Österreichische Ärztezeitung”.

Prim. Dr. Michael Smeikal, Dagmar Dehler, Prim. Univ. Prof. Dr. Peter Fasching, Susanne Domkar MSc. Dr. Georg Ruppe, Univ. Prof. Dr. Michael Hiesmayr, Univ. Prof. Dr. Regina Roller-Wirnsberger
Participants of the interdisciplinary expert panel (in alphabetical order):
Dagmar Dehler, Director Healthcare Nutrition DACH (Nutricia Milupa)
Susanne Domkar MSc., Country Manager Vienna – Association of Diabetologists of Austria / Working Group Geriatrics
Prim. Univ. Prof. Dr. Peter Fasching, 5th Med. Dept. with Endocrinology, Rheumatology, and Acute Geriatrics – Wilhelminenspital Vienna & President of AKE
Univ. Prof. Dr. Michael Hiesmayr, Med-Uni Vienna, Initiator and organizer of the NutritionDay
Univ. Prof. Dr. Regina Roller-Wirnsberger, University Clinic for Internal Medicine, University of Graz / Vice President of the ÖGG / Head of AK Nutrition in the AKE
Dr. Georg Ruppe MA, General Practitioner / Scientific Director and Managing Director of the Austrian Platform for Interdisciplinary Aging Issues (ÖPIA)
Prim. Dr. Michael Smeikal MSc, Haus der Barmherzigkeit Vienna; Center for Geriatric Medicine and Geriatric Nursing – Danube University Krems
Malnutrition in figures
Around 21% of seniors (65+) living at home are malnourished or at increased risk of it (1). 12.5% of hospital patients were considered malnourished in 2020. 18.5 percent were at increased risk for malnutrition. In nursing homes, this figure is as high as 28-53 percent of residents (2). The phenomenon of age-related nutritional deficiencies is increasingly becoming the focus of health care in an aging society. According to population projections, the proportion of people over 65 will increase to 26.4 % by 2040 (3). Malnutrition is partly responsible for increased morbidity and mortality (4), decreased functionality and quality of life, more frequent and longer hospitalizations, and up to 38 percent higher health care costs (5).
“Individuals who are elderly, lonely, and chronically ill are at an increased risk for malnutrition. Especially when the solitude is great, many people neglect their nutrition. You just have to ask people how they feel about their health situation, and they will tell you.”
Nutritional intervention reduces morbidity and mortality
If nutritional risks are present, a detailed medical history is essential. Countermeasures must be taken at the first signs of malnutrition, by rapidly initiating nutritional therapy. Data from the EFFORT study, published in the Lancet in 2019, show that systematically screening patients for malnutrition and providing nutritional therapy can have positive effects on the course of recovery. In this study, the targeted nutritional intervention significantly reduced mortality within 30 days. A 2019 meta-analysis of more than 6,800 malnourished patients found a 27% relative reduction in the risk of mortality up to 6 months after hospital discharge in patients who received nutritional intervention during their hospital stay. In a cohort study of more than 110,000 malnourished patients in hospitals, an analysis after exclusion of par/enteral fed patients showed that nutritional counseling or multimodal nutritional therapy reduced the risk of mortality by 25%.
“Screenings and subsequent assessments, as well as malnutrition therapy, should be established in the so-called ‘care pathway’ (Versorgungspfad) of the Austrian Social Insurance, as a part of the primary care sector in Austria. The Austrian National Nutrition Commission and the ONCA initiative supports this demand since 2012.”
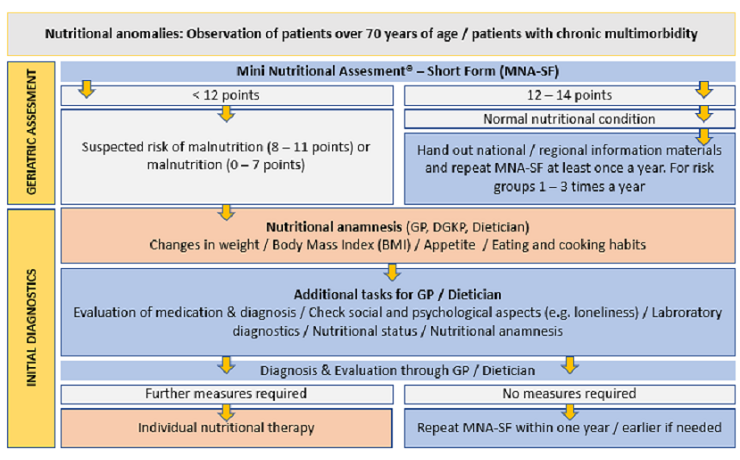
Care pathway (Versorgungspfad) of the Austrian Social Insurance
Recommendation: At least one screening per year
The panel of experts recommended that primary care physicians should routinely screen patients 65 and older at least once a year, preferably as part of their routine health checkups. In addition to recording weight, as well as calf and upper arm circumference, the risk of malnutrition can be assessed with simple anamnesis questions on appetite and quantity eaten, as well as a careful visual diagnosis. If a risk of malnutrition is identified, nutritional intervention should be started immediately.
“With simple questions that revolve around the appetite or the quantity of food eaten, as well as a careful visual diagnosis, the risk of malnutrition can be roughly estimated.”
Bringing dietology on board
Interdisciplinary collaboration is essential for successful intra- and extramural nutritional therapy. International publications demonstrate the added value of nutritional intervention, especially when dieticians work as part of an interprofessional team.
“Individual nutritional anamnesis, as well as therapy, must be in the hands of subject matter experts with appropriate qualifications.”
Oral nutrition supplementation can close nutritional gaps
Nutritional intervention using oral nutrition supplementations is becoming increasingly important in the prevention and treatment of malnutrition. Especially in cases of energy and nutrient (especially protein) deficiencies, high-calorie, high-protein medical sip feeds are an effective measure to close the resulting nutritional gaps. Replenishing the nutrient reserves can increase the physical and cognitive functions of patients and thus significantly improve their quality of life.
“An increase in protein and energy, for example via additional oral nutrition supplements goes hand in hand with an improvement in functionality and ultimately a survival advantage for malnourished patients. It is also a simple and cost-effective intervention.”
(1) Prevention Of Malnutrition In Senior Subjects in the EU, promiss-vu.eu
(2) Keller H et al. J Nutr Gerontol Geriatr. 2019 Oct-Dec;38(4):329-344.
(3) Bevölkerungsprognose 2020, Statistik Austria
(4) Gomes F et al. JAMA Network Open 2019; 2(11):e1915138
(5) Curtis LJ et al. Clin Nutr 2017 Oct;36(5):1391-1396.

Head of clinical medical nutrition, University Hospital Graz
Contact Julia for inquiries on Austrian campaign activities and for publishing of your Good Practice on this website.