Using data from a large cohort of renal transplant recipients, also including data derived from clinical practice, we found a considerable percentage of patients with reduced muscle mass.
We feel this is not only relevant for renal transplant recipients but is also likely applicable to other patient populations with complex chronic disorders, who may require a more in-depth nutritional assessment and monitoring policy to prevent underdetection of malnutrition and/or sarcopenia.
Routine monitoring linked to regular outpatient visits may further enable early and adequate detection of patients at risk and in need of multidisciplinary interventions.
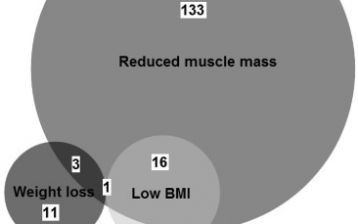
Over the last decades, the importance of low muscle mass indicating the presence of malnutrition and negatively affecting patient outcomes has been increasingly recognized. In the most recent diagnostic criteria for malnutrition by the Global Leadership Initiative on Malnutrition (GLIM), reduced muscle mass has therefore been included as a phenotypic criterion, in addition to low BMI and weight loss. A recent study using data from the TransplantLines Cohort and Biobank showed reduced muscle mass was the predominant (91%) phenotypic criterion for malnutrition in stable outpatient renal transplant recipients (RTR), and emphasizes the importance of routine monitoring of muscle mass in the care for patients with complex chronic disorders.
Malnutrition is known to be highly prevalent in nephrology patients, including patients on dialysis, but has not often been studied in RTR. The TransplantLines Cohort and Biobank was set up in 2015 at the University Medical Center Groningen (UMCG), The Netherlands, to increase insight in the health determinants and long term outcomes of solid organ transplant recipients. TransplantLines study visits are deliberately linked to regular outpatient visits and also use data derived from routine care, creating the unique opportunity to collect extensive data during a long period of time. These data provide us with new insights on the health of transplant recipients, with the goal to further tailor and improve patient care for this population.
In this recent study, we applied the GLIM criteria for malnutrition to a sample of 599 stable outpatient RTR. According to these criteria, 14% of patients was malnourished, of which reduced muscle mass determined by bio-electrical impedance analysis (BIA) was the predominant phenotypic criterion for diagnosis (present in 91% of malnourished patients). Importantly, the phenotypic criteria for low BMI and weight loss contributed little to the diagnosis, and 22% of malnourished RTR was overweight or obese according to BMI. Of the entire study population, 26% of patients had reduced muscle mass. We found similar results using creatinine excretion derived from 24-hour urine samples collected within routine care for the operationalization of the muscle mass criterion, however, the diagnostic value of this measurement still requires further investigation.
These findings underscore the importance of routine monitoring of muscle mass at outpatient visits for the assessment of malnutrition, and looking beyond BMI and weight loss alone. This may be of particular importance in patients with complex chronic disorders, in which assumptions on the stability of body composition are not met. Awareness is needed among health professionals for potential underdetection of malnutrition due to lack of muscle mass measurement in nutritional assessment. Accordingly, quick and practical tools for muscle mass monitoring in routine care are warranted. The current study is an example of how systematic evaluation of clinical data, both collected in study context and from routine care, can generate new leads on how to optimize nutritional care for all patients.
Clinical Nutrition Journal
Malnutrition according to GLIM criteria in stable renal transplant recipients: Reduced muscle mass as predominant phenotypic criterion
View article
BMJ Open
Rationale and design of TransplantLines: a prospective cohort study and biobank of solid organ transplant recipients
View articleThis project was a cooperation between the University Medical Center Groningen, department of Dietetics, department of Internal Medicine – subdivision Nephrology, TransplantLines Cohort and Biobank and the Hanze University of Applied Sciences. Contact: Iris M.Y. van Vliet, RD, i.m.y.van.vliet@umcg.nl or prof. dr. Gerjan Navis, g.j.navis@umcg.nl.