Welcome to Cambridge
The 2019 conference was opened by Professor Sumantra Ray, director of research in food security healthy and society at the University of Cambridge. He introduced us to some of the most notable research produced in Cambridge starting with the discovery of DNA by Watson and Crick. He moves on to discuss the excellent multidisciplinary work of the past seen in the partnerships formed by Elsie Widdowson and the medical team, highlighting partnership working between a dietitian and a doctor. Cambridge University is famous for interdisciplinary working and trying to find solutions to chronic problems in a world of ever diminishing resources. Supported in the UK by an NHS the is now reprioritising nutrition Professor Ray suggests we now in a position with properly placed nutrition in healthcare to make key changes.
The Trinity: Patients, Professionals & Decision-makers

Lord Lansley
What do politicians need to know and how can politics help further improve person-centred nutritional care?
Lord Lansley
House of Lords
Lord Lansley opens by describing his position as both a policymaker and a patient, having recently experienced bowel cancer. He talks about being thankful for being able to eat, and his experiences supporting his elderly mother who wanted to eat but was unable to. He describes the profound effect it had on him as a policy maker. Lord Lansley acknowledges the challenges of constantly being offered food and the reaction of people to his large weight loss of 17kg over a year. Lord Lansley was grateful for his access to a dietitian and nutritional advice. Most notably for him, his starting advice was no fibre, eat crisps and marshmallows.
Lord Lansley describes the “Complex relationship that humans have with food”. He describes the government’s acknowledgement of the prevalence of malnutrition and the commitment to better screening for malnutrition and better standards of food in hospitals. The change that followed was a review of hospital food. The result is not fundamentally about malnutrition in hospitals but about the food, which is less beneficial for patients who cannot eat at all. He describes the focus as still on obesity and not yet balanced with malnutrition. He hopes we can move to combat malnutrition and obesity at the same time. “We need to give people access to food and that is a societal challenge”.
Lord Lansley finishes by acknowledging the need for leadership to support improved outcomes. He suggests that we need to audit current procedures then focus on specific elements to get the desired outcomes. He quotes the reductions seen in cases of Clostridium difficile when this was an NHS focus. This leads to a need to update commissioning guidance. He would like to know if patients receiving treatment from the health service actually recover, their nutritional status and the acknowledgement that in many cases, it is worse.

Ben Howlett
The new health and social care landscape in the UK: opportunities to
improve nutritional care
Ben Howlett
Managing Director Public Policy Projects
Most important policy papers
Ben Howlett opens by talking about one of the most important policy papers, the 2019 NHS Long Term Plan. The 136-page document only mentioned nutrition 5 times. Ben suggests it may be missing from the bigger picture. Furthermore, The Advancing our health: prevention in the 2020s consultation document suggests the predominant issue is obesity, particularly childhood obesity, suggesting a lack of understanding from the government. Ben suggests that there needs to be more acknowledgement of the scale of the problem – 1.3 million people over 65 are suffering from malnutrition – 93% our in the community.
Ben highlights some potential opportunities for improving healthcare including the general election 2019, the current reforms in the landscape of health care and our ageing population. He makes reference to the document “The importance of nutrition
to the integrated care debate” which recommends better nutrition practice, data collection, education and training alongside a whole system approach. He finishes by highlighting that outreach is needed for solving problems in malnutrition. Changes are needed in acute trusts that can be taken into the community.

Trevor Smith
BAPEN, PINNT & UK Malnutrition Awareness Week: Good Practice in multidisciplinary collaboration
Trevor Smith
President of BAPEN
Empowering people to take responsibility and self-screening for malnutrition risk.
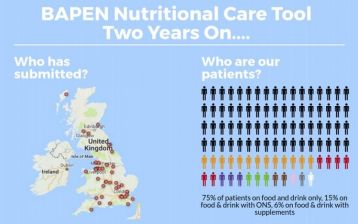
BAPEN president, Trevor Smith is a Consultant Gastroenterologist working in Southampton where he leads a clinical nutrition and regional intestinal failure service. He opens by describing the purpose of BAPEN as a multi-disciplinary charity which aims to think upfront about where patients fit, with outcome-based structures for nutritional care.
He describes the success of Malnutrition Awareness Week (MAW2019) which took place between 14-20th October 2019 in combination with the Malnutrition Task Force, strongly supported by Age UK. There was a 389% increase in reported screenings from 2018-2019. There was also widespread media and social media coverage. Trevor highlights that it is common to often forget the consequences of malnutrition with the belief that this is a normal part of ageing. He urges us to challenge that belief.
Trevor continues by describing disease-related malnutrition, which is not always just relevant to those who are elderly. He comments on the lack of nutrition in medical training meaning some practitioners, for example, those working in COPD have no idea of nutritional requirements.
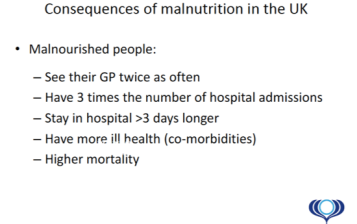
Consequences of Malnutrition
Trevor Smith finishes by sharing some nutritional statistics related to malnutrition
• 5% of the population have disease-related malnutrition
• Individuals with malnutrition – 93% free-living, 5% care homes, 2% hospital.
• 1 in 10 older people are suffering from or at risk of malnutrition

Caroline Wheatley
Empowering people on home artificial nutrition to take responsibility
Caroline Wheatley
Chair of PINNT, BAPEN executive officer and a patient of parenteral nutrition.
Caroline opens by describing the role of PINNT (Patients on Intravenous & Nasogastric Nutrition Therapy) as a mechanism of Support, Education and Collaboration.
She describes how guidelines and documents are often overwhelmingly large and therefore not user-friendly for patients which let to PINNT re-creating them as A4 flyers that are useable for the patient. She highlights the importance of these documents as they contain standards that make key promises to patients. The documents relate to clinical care and patients often have no awareness of what they are entitled to. Caroline challenges us to consider if patients are aware of clinical and quality standards and furthermore if clinicians know? One of the PINNT’s roles is to frequently challenge when these promises not being kept.
Caroline takes us through the patient’s journey as they move between the hospital (dependent) to home (independent). Relevant to empowering people and assume responsibility.
PINNT in collaboration with BAPEN will survey patients on home enteral feeding in January 2020. The results of which will form a workstream. The results of this survey will inform a 2020 workstream to ascertain if the NICE Quality Standards – Nutrition Support in Adults (2012) are being adhered to.
PINTT takes steps to all patients to feel empowered to have nutrition wherever they need. They have developed a medical tag to identify that essential medical equipment is being carried.

Monika Malickova
Are the needs of individual patients being met?
Monika Malickova
PN patient from the Czech Republic, head of the International patient group PACIFHAN (International Alliance of Patient organisations for Chronic Intestinal Failure (IF) and Home Artificial Nutrition (HAN)
Monika opened with her experience as a patient who has required long term artificial nutrition. Following on from this she introduced us to the 9 countries that are currently members of PACHIFAN including Denmark, Sweden Italy and the UK.
As an organisation PACIFHAN aims to be a trusted international reference on HAN from a patient’s perspective, encouraging peer-reviewed research. Further aims include an increase of awareness and quality of life for HAN patients. PACIFHAN also aims to tackle areas where patients feel their needs have not been met, including training and access to equipment.
Monika closes by inviting us to take part in and promote World Home Artificial Nutrition Day on 15th October 2020.
Key note debate patients, key opinion leaders and conference delegates


The following questions were posed to the debate panel following this mornings session.
What is the driver of the agenda for the decision-makers? What is the media doing?
What will get through is the relationship between malnutrition and poor care in the elderly? For politicians, that is where this starts from, it is quite difficult to get into wider groups. There is a serious debate in how many older people are malnourished and wider outcomes on co-morbidities. Politicians need to move on from how we fund social care to the quality of what is being provided.
Are we spending the money the right way?
Understanding how the NHS works, a managerial factor is that managers are inclined to measure the marginal cost and not the cost-effectiveness. Building issues relating to nutrition into the way in which health care systems manage themselves is very important. CCG – thinking about the overall effectiveness of your budget – reflection on the costs incurred. Tariffs for treatment program – doesn’t show any evidence that the cost structure includes support for nutrition – this should be challenged. Display where savings can be made.
What would be the most important data to collect?
1. Research – Connected diagnosis across the world. Working together to create collaboration.
2. Direct – NHS health checks for the wider population is underutilised and not been updated for a long time.
Patients would like to collect information on QOL. Investment of the patient and not just a clinical investment.

sweet, sour, bitter, salty and umami flavours
Optimal Lunch for All
We are introduced to lunch where butter and oils have been prepared in a series of sweet, sour, bitter, salty and umami flavours. We are able to add specific flavours to our meal’s dependant on our own tastes. The taste test initially developed to support oncology patients allows the chef to create a specific taste profile to each person.

Salutations by Rocco Barazonni, ESPEN chair

Annemieke van Ginkel, EFAD president
Salutations – Annemieke van Ginkel, EFAD president & Rocco Barazonni, ESPEN chair
Annemieke opens up the afternoon session by introducing to EFAD (European Federation of the Associations of Dietitians), which currently represents 32 National Dietetic Associations and 39 educational associate members. The 2019 EFAD white paper Sustainable Health Through Life Span: Nutrition as a Smart Investment for Europe makes a case for dietitians and highlights that dietetic interventions demonstrate statistically and clinically significant impacts on health outcomes. Furthermore, Annemieke describes how the white paper calls for more inclusive of nutrition in health care outcomes and more collaborative working.
Annemieke moves on to describe the financial impact of dietary intervention, with research suggesting for every €1 of dietary counselling providing society with net benefits of €14 or €63 over a five-year period. Malnutrition is reported as having double the economic cost as overweight and obesity. Finally, Annemieke describes the European dietetic action plan which was developed to highlight how dietitians are implementing the WHO Food and Nutrition Action Plan.

Frances Healey
Patient safety in nutritional care
Dr. Frances Healey, Deputy Director Patient Safety (NHSI/E)
Dr Healey shares how the national Patient Safety Team identifies incidents and shares learning to address problems and prevent further re-occurrences. She describes the various agencies involved in patient safety including the CQC, MHRA and NHS Improvement Estates and Facilities.
Dr Healy shares the national learning resulting in safety improvements for nasogastric tubes, including changes in technique and equipment. She highlights the technique of air auscultation was removed in 2005, however, the same technique in the USA resulted in the death of an infant, suggesting a lack of international collaboration.
Dr Healy moves on to discuss an incident where an NG tube is placed, unable to aspirate, the doctor confirms position via CXR and initiates feeding, the tube was placed in the right main bronchus resulting in clinical complication. She highlights that medical staff are often given training after an incident, however, there is a need for more training in advance. The creation of the International Dysphagia Dietary Standards Index (IDDSI) was created to reduce the translation gap between expert and everyday understanding by standardising procedures. She completes her session with a quote from Terry Pratchett “There have been times, lately, when I dearly wished that I could change the past. Well, I can’t, but I can change the present so that when it becomes the past it will turn out to be a past worth having.”
Updates from Paris, keynotes and plenary debates 4 content tracks by patients and professionals

Measure | Prevalence and Economics studies
Update: Pavel Těšínský, Czech Republic
The importance of measurement: Evidence and research are the basis for everything
Pavel opens with the statement, “malnutrition is a problem”. He describes how it has been recognised, named, defined, consequences identified, impact measured but we are working on a solution. He points out that malnutrition is a problem – even in highly developed economies.
Pavel Těšínský
The World Health Organisation definition is – “a world free from all forms of malnutrition where all people achieve health and well-being” Pavel suggests that in order to tackle malnutrition is needs to be a task for society, politicians and the public. The target is to spread information and to put malnutrition on the public health agenda.
In order to measure the overall impact of malnutrition, we use a series of measurements.
1. Validated screening tools to identify malnutrition include, MUST, MNA, and NRS2002
2. Economic considerations highlight the cost of disease related manutrition and economic considerations in the use of medial nutrition. Malnutrition is a major public health issue.
Once we have this information, we need to successfully communicate it through science, practice, politics and the media.
Pavel suggests that we need to present malnutrition as the major and costly problem and establish optimal nutritional care as a cost-effective solution.

Educate | Nutrition in Medical Education
Update: Cristina Cuerda, Spain.
We are introduced to the ESPEN, NEMS project – Nutrition Education in Medical Schools. Data collected through ESPEN, ONCA and academic institutions was published in 2017 followed by a position paper in 2019. The survey identified the themes on basic nutrition, clinical nutrition and applied nutrition taught in medical schools.

Cristina Cuerda
Opinions were sought on the key factors to successfully implement human nutrition curriculum in medical schools. As a result, the basic knowledge that should be taught in medical schools was established. The next step for the project is implementation – with a meeting planned in January 2020.

Gaston Remmers
Patient versions of nutrition guidelines
Keynote: Gaston Remmers (Cees Smit)
Gaston introduces us to the European Patients Forum (EPF) and the activities they have undertaken since 2013, staring with the publication of the book “Patient Perspective on Nutrition”. In 2018, a patient task force was created. Formal collaboration with ESPEN in 2019, increased patient involvement in guidelines development and summaries. This patient involvement will result in the creation of lay versions of current guidelines. At present, ESPEN is contacting interested patients and forming working groups for 14 key themes.

Implement | Nutritional care in hospitals and the community
Update: Elisabet Rothenberg
Elisabet introduces us to Senior alert – A national quality register for preventative care of older adults in Sweden. As a part of this process, they have been able to highlight that malnutrition needs

Elisabet Rothenberg
CNA – consulted on the definition of national food policy, involved in 83 policies including food in hospital and food and health.

Maarten Soeters
Implementation strategy, organizational awareness & execution
Maarten Soeters – Amsterdam UMC
Maarten introduces us to his work on an inpatient hospital setting in Amsterdam. In 2017, the patient’s voice
representative from patient boards requested that nutrition be changed.
Patients wanted better food, taste choice and flexibility of eating schedules. Alongside these healthcare professionals needed to ensure that food met safety requirements, optimal intake and therefore good outcomes. Some of the key things implemented from this consultation are ordered at short notice, measuring intake, sustainability, patient-directed menus and 6 meals per day. To evaluate the program, they follow the pathway plan, do check, act. More scientific research is planned through the use of breakfast buffets to provide more personalised nutrition.
Maarten highlights that altering the composition of the food, i.e. to increase the protein content is not useful if the patient chooses not to eat the food offered. Therefore, we need to be looking at the taste, the food on offer and patient satisfaction alongside nutritional content. He champions the use of multi-disciplinary team including the patients to implement new nutritional policy in hospitals.
Influence | Influencing public awareness and policy
Keynote: Rachel Power: What are routes for patients to make their voices heard
Rachel Power is the chief executive of the Patient’s Association and she starts by introducing us to their key values of compassion, collaboration, inclusion and empowerment.
We are asked to consider the question of why patients need to be empowered?
Rachel reports that when patients are empowered, we have better physical and mental wellbeing, improvement in services, maximise impact, promote inclusivity and respond to change. The Patient’s Association has a helpline that gets around 3500 calls and a range of projects for the patient voice.

Aníbal Marinho

Rachel Power
There are many ways that healthcare professionals can work with patients. Equal partnerships with patients, excellent communication, information and support, and finally acknowledging patients’ thoughts and needs lead to a valued patient experience. Rachel’s take-home message is that patients do not want a “good” service but a great service.
Co-creating the patient pathway

Joost Wesseling
Follow up Paris Spring Meeting: Outcomes ONCA survey
Joost Wesseling, European Nutrition for Health Alliance
Joost introduces us to the results of the ONCA survey following on from the Paris spring meeting 2019. 84 responses in total covering a wide range of professions and patients, from 28 countries (18 ONCA countries).
They identified the main elements of a frictionless nutritional pathway as education, evidence-based practice, MDT, integrated nutritional care pathways and screening. The consensus was that during the patient pathway nutrition should be introduced as early as possible and a lack of nutritional advice could be a bottleneck to that frictionless pathway.
In regard to measurement, 75% of respondents felt that the proportion of patients who have been screened for malnutrition and the goals within the medical diagnosis would be the best indicator of quality. The resulting benefits including quality of life and health outcomes. Respondents concluded that education for all parties was essential to contribute to this nutritional pathway, with an emphasis on shared responsibility.

Rebecca Stratton
Integrating nutritional care into the patient pathway across health and social care systems: Why and how?
Dr. Rebecca Stratton
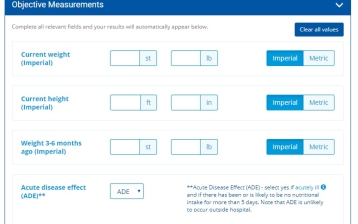
Dr Rebecca Stratton, the chair of the Malnutrition Action Group, British Association for Parenteral and Enteral Nutrition (BAPEN) introduces us to the benefits of integrating nutritional care for malnutrition into the patient pathway. Dr Stratton starts by highlighting why we should integrate – improving identification of malnutrition leads to the right nutritional care to improve outcomes, primarily benefitting patients but also saving money and therefore benefitting society.
She informs us that there are 5000 uses of the MUST tool per month on the website. Better identification can be seen through Integrating these tools into hospitals and NHS software packages. Furthermore, we need to move towards embedding decision making and management pathways into disease-specific guidelines. In regard to raising awareness, she re-iterates that dietitians need to be the voice, empowering other professionals and patients to act.

Marek Lichota
Experiencing a patient Pathway
Marek Lichota, Apetite for Life
Marek describes the experience he underwent as a patient who becomes reliant on parenteral nutrition. After illness and surgery, he found himself malnourished and unwell before he reached the point of a nutrition assessment. Marek argues that his journey, in a linear fashion does not support the patient in the most successful fashion. By having a tool that integrates with technology, through social networks, patients will have faster access to specialist treatment and their supporting medical professionals can get up to date reports from patients. Engaging patients with new technology puts them in the middle of healthcare.
The Digital health record is reported as a convenient way for individuals to control their own health, with individuals using the record rating their care and the care available as good, very good or excellent. This is echoed by healthcare professionals who reflect on the positive impact of having data related updates. Finally, Marek highlights some of the new technologies working to improve infection control. Care coordination, supply management, referrals and patient experience.

Pawel Kabata
How can we learn from a (Digital) Customer’s Journey
Pawel Kabata, MD, PhD, Consultant oncological surgeon, Assistent Professor, Department of Surgical Oncology, Medical University of Gdansk
Dr Kabata introduces us to himself as consultant oncological surgeon, assistant professor and certified clinical nutritional professional before introducing his alter ego who has 38k followers on social media. Dr Kabata is engaged in health promotion and education. He talks about the Patient digital pathway, where technology meets medicine. He refers to patients willingness often to following advice and even self-diagnose from Google, yelp, YouTube and even Facebook.
We need to be on social media to influence people in the correct way. 63% of patients will trust a professional with a strong online presence. Dr Kataba highlights some of the benefits of social media such as providing direct viewer feedback and real-time engagement. It provides an opportunity to network and to build solid relationships.
An #instadiet study of 5 popular hashtags #nutrition, #nutritionist, #diet, #dietitian and #instadiet found a total of 1250 posts. 93% of those Instagram posts were poor. Dr Kabata describes Instagram as a “giant cookbook with a slight coaching vibe”
Our responsibility to provide people with good-quality data that is well controlled. We need to be a resource as medical professionals and be willing to educate. Through our different specialities, we can use our wide reach and experience to provide good, sound advice through social media. He encourages us to use our influence to make a difference.

Aníbal Marinho, APNEP

Dinner at University Arms Ballroom
DAY 2
THE INTERACTIVE SESSIONS


Harrison Carter
Dr Minha Rajput-Ray and Dr Harrison Carter: Nutrition Education in Healthcare Practice: Implementation Pathway Project
The second day of the conference started with a talk from Dr Minha Rajput-Ray and Dr Harrison Carter on behalf of the NNEdPro Global Centre for Nutrition and Health think tank specifically highlighting their focus on the need for strategic partnership between disciplines and keeping patients and carers at the core of their research.
A large focus of their talk focused on their ‘Junior Doctors Study’ carried out in 2018 in which 20 trainee doctors were surveyed to explore their observations and attitudes on current nutrition care in Addenbrookes Hospital (Cambridge) to identify possible gaps in the management of hospital malnutrition and lack of training.
They shared some very interesting results, most notably that there was agreement amongst the Junior Doctors about the importance of nutrition in health and appreciation of the doctor’s role in nutrition care and it was felt that there was need for a multidisciplinary approach to achieve this. They reported their nutrition training to be inadequate with a resultant lack of confidence in their nutritional knowledge. One of the most interesting findings was that the Junior Doctors identified Consultants as those best placed to promote nutrition. The main conclusions drawn from the study were that doctors are likely to engage positively with increased nutrition training if the ideal method for its provision can be established and also that Consultants may have a role to play in raising the profile of nutrition care among trainee doctors.
They then spoke about their ‘Patients and Carers Sub-Study’ which focussed on the patient and carer voice. This revealed that half of the participants had never spoken to a Doctor about food or nutrition as felt there was no point in doing so. There was also a belief expressed that Doctors don’t have the knowledge or time to advise patients on food. It was felt that nutrition care in hospital is often Doctor led and so if the Doctor doesn’t mention anything to do with nutrition, the patient and/or carer doesn’t either. It was expressed that they did not feel Doctors could do anything about the quality of hospital food. Perhaps most importantly, it was reported that patients and carers who were provided with nutritional advice often could not follow it due to a lack of understanding of the technical terms used and a lack of guidance on actual food choices especially in conditions which affected their intake.
They then introduced their current and future projects including the ‘Nutrition Implementation Coalition’ which aims to broaden the conversation about nutrition in health for the benefit of the patient through various means including increasing the nutritional knowledge within health professionals’ curricula. They are also in the process of writing a book: ‘Elsevier Essentials of Nutrition in Medicine’ and are also working on parliamentary policy dialogue on raising NHS Food and Nutrition standards.

Clare Shaw
Dr Clare Shaw: Essential steps in the Nutritional Care Process
Dr Clare Shaw spoke about the essential steps in the Nutrition Care Process (screening for malnutrition, nutritional diagnosis, nutritional assessment and targeted individualised nutrition intervention).
She spoke about the need for nutrition screening to be sensitive and specific so that those at risk of malnutrition are identified and those who aren’t being ruled out. She also highlighted that tools used for screening should be validated and that there must be good training in using these tools to ensure their effective implementation. However, she emphasised that criteria for referral to a Dietitian should be broader than just a screening tool.
It was stressed that identifying a person as at risk of malnutrition is only the first step and once a person is identified, the causes of malnutrition must then be identified. She suggested that using a framework may be helpful such as the Patient-Generated Subjective Global Assessment or the ESPEN GLIM criteria.
The British Dietetic Association’s ‘Process of Nutrition and Dietetic Practice’ was described as an ideal framework to underpin how malnutrition is managed as it allows a thorough nutritional assessment to be performed and allows for targeted and individualised interventions to be used due to its service user focus.
Finally, Dr Shaw emphasised the need for nutritional care to be provided by the multi-professional team.
Good Practices Exchange Market

After the two talks, the focus changed to the ‘Good Practice Exchange Market’ which was designed to elicit good practices from round table discussions. It provided an excellent opportunity to learn from delegates from other countries and gain an understanding of what others were doing to enhance the nutritional care provided. There was noticeable enthusiasm for this amongst delegates.

At the end of these discussions, a table leader was elected to present the top three good practices which provided an insight into just how many good practices there are in nutritional care throughout the 18 member countries and highlighted the importance of sharing these. It was also beneficial in terms of raising awareness of the weekly Good Practices page on ONCA’s website so that members can continue to learn and take inspiration from other members’ innovative and patient-centred initiatives. The good practices shared by delegates on the day were captured and will shortly be published on the Good Practices page.
How can we develop the campaign to serve individual EU patients’ needs & drive self care

The next part of the interactive sessions focussed on how the ONCA campaign could be further developed. Delegates were allocated to another table where they brainstormed ideas, strategies or activities which could be used to accelerate the campaign.

Different tables discussed 1 of the 4 ‘Key Content Tracks’ used by ONCA to explore Good Practices: Measure, Educate, Implement and Influence. The outcomes from these discussions will be used to inform future strategic development within the campaign.
Many suggestions were shared, including:
- widespread publication of data to increase awareness of the benefits of good nutritional care
- raising public awareness of malnutrition
- recognising the value of social media in presenting the correct messages
- educating the healthcare professional workforce on nutrition
- generating joint recommendations for different professionals endorsed by their professional bodies
- aligned training portal and certification for healthcare professionals
- having a champion for each country to channel best practice ideas
- having greater patient involvement of the ONCA website
Output interactive brainstorms to further develop the campaign’s four content tracks
190.75 KB
Download
Optimal Nutritional Care for All events 2020 & strategy 2021-2023
Frank de Man and Joost Wesseling presented on planned activities for 2020 including:
- growing the campaign both in terms of members and use of good practices
- greater emphasis on engagement from Nutrition and Dietetic and medical students in using the Good Practices website page
- leveraging patient versions of nutritional guidelines
- lobbying the European Parliament to leverage ONCA objectives
- development of a campaign masterplan
- welcoming new member countries into the campaign
KØBENHAVN CONFERENCE 2020
Finally, The Optimal Nutritional Care for All 2020 conference in Copenhagen was introduced which will focus on ‘Creating Equality in Nutritional Care’ and will take place on the 23rd and 24th November 2020.


Summary by Trevor Smith, President of BAPEN