The Amsterdam OPTIMAL NUTRITIONAL CARE FOR ALL conference. Continuity of nutrition care: the power of concerted efforts against malnutrition
G.M. van der Werf1,2,3, C. van Dronkelaar4, M.F.M. van Stijn1,5
1 NESPEN Clinical Nutrition and Metabolism, the Netherlands
2 Amsterdam UMC location University of Amsterdam, department of Endocrinology & Metabolism, Meibergdreef 9, Amsterdam, the Netherlands
3 The Hague University of Applied Sciences, Faculty of Health, Nutrition & Sport, The Hague, The Netherlands
4 Centre of Expertise Urban Vitality, Faculty of Sports and Nutrition, Amsterdam University of Applied Sciences, Amsterdam, the Netherlands
5 Amsterdam UMC location University of Amsterdam, department of Anesthesiology, Meibergdreef 9, Amsterdam, the Netherlands
Summary ONCA day 1:
Opening by the chairs:
Mireille Serlie
Professor Of Medicine; Nutrition and Energy Metabolism at the University of Amsterdam
In this conference, 22 countries are participating. It is important to have the discussion about ‘Optimal Nutritional Care for All’. More and more older people are living in the Dutch capital, it is expected that 16% will be 65+ in 2030, many of whom are suspected to be malnourished. Approximately 21,000 malnourished older people will be living at home in 2030. In the Netherlands, we are not ready for this, but we can prepare ourselves through discussion and by learning from each other. Collaboration between policymakers, patients, and healthcare providers is essential.
Olle Ljungqvist
Professor of Surgery at Örebro University Hospital
Knowledge and science must be translated into policy via a PAN European approach. ONCA alliances are starting the conversation in every country, integrating the EU agenda within the national agendas. In addition, recently Hungary joined as well, making it the 20th country to join ONCA. ONCA makes an impact by sharing good examples and making them applicable to every country. A lot has already changed at European and national levels. Let’s fight together for the right nutrition for the older, the weaker, and the patients.
Session 1: Continuity of nutrition care: the power of concerted efforts against malnutrition in Europe.
Marian de van der Schueren
Professor of Dietetics at Wageningen University & Research and Professor of Nutrition and Health at HAN University of Applied Sciences
Nutrition Science and policy at glance
Malnutrition is not only a problem for underweight people but also for obese people. The fact that we are getting older, living longer at home, but also with more comorbidities raises challenges. Malnutrition is also increasing in older adults living at home and this is a multifactorial problem (DoMAP model). Examples include lower food intake, higher nutrient needs, lower bioavailability of food, but also many symptoms of disorders that lead to malnutrition. Malnutrition leads to disease, and it is therefore important to be recognized as soon as possible and action should be taken. Another challenge is the shorter length of stay in hospitals (in NL this is 3.5 days). People recover at home, but the question is whether this transfer is properly arranged, and do we have the resources to do so. A next challenge is the rise of eHealth. Although eHealth offers opportunities it also comes with problems like no communication between different care platforms and that many apps have not been validated. But also, the willingness of participants to use apps should be taken into account. Healthcare costs are rising fast (+2.9% per year in the Netherlands) partly due to advanced age, medical technology, larger population, the costs of cancer and it is striking that ‘women cost more’. Obesity brings additional challenges, especially sarcopenic obesity and in the context of malnutrition. This is not yet recognized despite initiatives to make it more known.
Fortunately, there are also opportunities. For example, the arrival of the GLIM criteria, on which more than 300 articles have already been published. Speaking the same language creates opportunities to tackle malnutrition in its early stages and makes policy formulation easier. Work is now being done on the GLIS: Global Leadership In Sarcopenia, which focuses on protein intake, exercise, screening, control of inflammation, and stress reduction. An additional opportunity is lifestyle as medicine, so nutrition and exercise become the primary treatment. Challenges are also being created in policy, for example, the WHO has a plan to stop obesity and malnutrition is being discussed within the ICD-11. The Integrated Healthcare Agreement in the Netherlands has also been developed, which strives for accessible and affordable healthcare, in a home setting, when possible, with an increased role for digital support and better interprofessional collaboration. We need to focus on health rather than the disease. Because food is relatively cheap and easy to apply, this is an important focus point. The food train is running, there are many opportunities, so jump on this train!
Mark Nuijten
A2M- Minerva HE Network , Business Valuation Erasmus University Rotterdam
A pan-European approach to nutrition economic research:
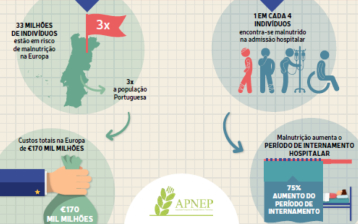
By quantifying the effect of the burden of disease, the effect of malnutrition and, above all, the effect on quality of life and the costs for society, policy can be made. For each healthcare setting, the clinical consequences and the effect on quality of life must be made transparent, as this leads to economic consequences. In policy, the main aim is to achieve a major impact of treatment, fewer complications, shorter admissions, cost-effectiveness and a better quality of life. This can be made transparent by QALYs: a cost-benefit analysis that makes the economic assessment between the effectiveness and the costs of a healthcare treatment, expressed in an extra year of life in good health. Because food is relatively cheap and can yield a lot of health benefits, it produces many QALYs compared to medicines, for example. Food therefore provides many QALYs with lower costs. This should be communicated to policy makers. A pan-European approach which consists of one basic model which can be tweaked per country allows for comparison between outcomes across countries. This creates opportunities to learn from each other. An example of a cost-benefit analyses showed in the Netherlands that 10-20 million euro could be saved per year when malnutrition would be treated.
Manuel Arellano
Patient advocacy. Kidney patient involved in improving the quality of life of people with chronic disease or disability. Volunteer on boards ALCER, COCEMFE, CERMI, POP, EPF
The role of patient advocacy in the European debate
There are 78 patient organizations in Europe, representing 150 million patients across 19 countries, currently represented by EPF. They strive for good identification of patients at risk, good use of assessment tools, primary prevention and prevention of multi-morbidity. This starts with the training of healthcare workers. They must identify risks, discuss the effect of nutrition when diagnosing illness, inform about the importance of nutrition and design guidelines. No one knows the patient better than the patient, he/she is co-responsible, so he/she needs good information about the possibilities. It is important to ask the patient what is important to him/her and to report PROMS (=Patient Reported Outcome Measures) and PREMS (=Patient Reported Experience Measures) in studies alongside clinical effectiveness.
Because many patients are often unaware of malnutrition, available and clear information is essential. Not only in text but also visually. In addition, support, personalized diets, and care for informal caregivers are essential. It is important to talk to the patients and not to think for them about what they need. It is difficult for the patients to assess the value of all information and to find good or correct information. Many patients do not like that everything is provided digitally but prefer to engage in conversation. Active patient participation and empowerment is most important as their experiences are a vital measure of the health care quality. So put the patient first and discuss his/her options as the patient is a person first and not a disease.
Marjolein Visser
EuGMS. Full Professor at the Vrije Universiteit Amsterdam
Creating European awareness of the role of nutrition care in geriatrics: an inventory of successful initiatives.
Malnutrition in the elderly is poorly recognized in primary and social care. Due to lack of recognition, there are more negative consequences. Malnutrition starts at home and in Europe 95% of the elderly live at home. In addition, older adults themselves often have poor awareness of malnutrition. Because malnutrition is not sufficiently under the spotlight, little screening is done by health care professionals. Also, nutrition is not part of medical curricula. The subject seems avoided due to the lack of knowledge. The focus is now often on overweight. Also, not all elderly people go to their general practitioner, they are not aware of the risk of malnutrition and see it more as a problem for poor countries or in war zones. Weight loss is considered normal or even desirable. And this leads to negative consequences. What can we do about this? By creating and monitoring awareness, incorporating nutrition into medical curricula, giving courses, approaching subgroups, referring to dietetics, mandatory screening, and involving welfare workers, we are one step closer to a desirable situation. All this in co-creation with the patient and his family.
The Malnutrition Awareness Scale (MAS) is a 23-item questionnaire which the patient completes themselves within 10-20 minutes. It measures awareness objectively, identifies subgroups where awareness is less and evaluates interventions. The MAS is based on the I-change model. The word malnutrition is not used within the questionnaire because it evokes many negative associations, the GLIM offers an alternative. However, the term unintentional weight loss was also not understood. It was striking that when the MAS was deployed, 25% of the population did not see hospitalization as a risk for malnutrition. Lower SES (socio-economic status) and older age were also risk factors for less awareness. Overall, the MAS can help to increase awareness on malnutrition among older adults as well as health care professionals and social welfare workers.
Maria van den Muijsenbergh
EFPC. Professor of Health disparities and person-centered integrated Primary Care.
Primary care and nutrition: how can the European Union help?
We must provide personalized primary and specialized care to the home situation of patients. Due to multi-morbidity, multidisciplinary work is becoming increasingly important, and the dietician must be involved in this. We need to work more goal-oriented than disease-oriented. When health care is driven by needs and values, the patient and society feel more involved. This leads to better outcomes, independence, and lower healthcare costs.
The patient is the expert of his/her own life, and many factors influence this, which means that everyone’s goal is different. It is therefore important to include social and living environment, food choice and eating habits, communication, barriers in quality of life, anthropometric data and movement pattern in the considerations, in multidisciplinary team approaches and with assessment of the process.
Continuity of care must also be taken into account. This requires better communication and referral to the primary care. The patient wants to build a relationship with his care provider, this can be done by working on a care circle with continuity of information, relationship and management in collaboration with others. Good examples are patient passports (The Netherlands), the Home Enteral Nutrition Service (UK) and shared patient records (Estonia).
Panel debate: What are actionable recommendations to improve the continuity of nutritional care in our health systems.
Arthur van Zanten (NESPEN), Robert Greene (Global Oncology Patient Advisory Board), Annemieke van Ginkel-Res (EFAD), Rocco Barazzoni (ESPEN), Maria van den Muijsenbergh (EFPC), Marjolein Visser (EuGMS), Manuel Arellano (EPF)
The challenges in nutritional care are the transfer between all layers of health care, awareness, impact on quality of life, and the risks that malnutrition entails. To be able to provide good care, stratification will have to take place. At the policy level, we need to step out more and enter into dialogue with politicians.
However, patients and healthcare providers must first face the risk themselves, including non-obvious healthcare professionals (i.e., dentists). General practitioners can also play a role in this. It is an interdisciplinary problem, in which collaboration, shared decision-making, referral, research, implementation of research, and more support for primary care is essential. The first step is recognition, followed by cooperation (also with the patient and patient organizations) and information provision. We still have a long way to go but being at this conference helps!
Session 2: Good practices: Supporting the implementation of European policies and guidelines.
Alessandro Laviano
Associate Professor at Sapienza University of Rome
Europe’s Beating Cancer Plan: Integrated Nutrition Cancer Care: drivers for successful local implementation
60 years ago, cancer became a global threat, and survival was seen as the most important outcome. Nowadays, mortality has decreased in almost all cancer types. The diagnosis is made faster, which improves life expectancy and makes cancer a chronic disease. Survival therefore might not be the best measure for cancer patients anymore as survival addresses the tumor and not the patient. Quality of life is key in chronic disease and has been reduced by limitations in physical ability during and after cancer treatment. Sarcopenia is the main driver for a poor quality of life. Nutrition is important for optimizing the quality of life. There needs to be a shift from treating disease to achieve survival to improving quality of life. Costs must be taken into account because the economic impact of treatment is extreme (1 trillion dollars for cancer treatments per year), this is not sustainable. We need to consider treatment-associated toxicity more, is it worth it? Compared to research, medicines are a lot less effective in real life. By focusing more on the patient, complaints (such as severe fatigue) are recognized more often. Nutrition can support the treatment’s efficacy and help with associated complaints, given that this is tackled integrally. Oncological treatments must be personalized, patient-reported outcomes must be discussed and the importance of nutrition must be communicated. Highlighting the unmet needs is key to successful implementation.
See also: Policy Brief, nutrition care is an integral part of patient-centered medical care, a European consensus. What are the next steps? https://doi.org/10.1007/s12032-023-01955-5
Integrated Nutrition Cancer Care: Informing Policymakers for Better Health Outcomes
Press ReleaseMaarten Soeters
Endocrinologist MD PhD – Endocrinology & Metabolism – Academic Medical Center Amsterdam
Targeting Malnutrition: from Awareness to Control.
Do we see the elephant (malnutrition) in the room (or tulip fields) and are we aware of the consequences? Everyone has an opinion about food, but no one takes responsibility. In the Netherlands, nutritional care is well organized and substantial investments are made. Malnutrition is recognized through the use of quality indicators, the week against malnutrition, the ‘Leerboek Voeding’ and the (social) media attention. However, awareness is not yet control, there are no parties who are hold accountable yet. The control (accountability) of malnutrition must become as normal as hygiene rules in hospitals in the light of infection prevention. This starts with the training of health care employees and by putting dieticians in the lead.
Michael Hiesmayr
Prof. Anesthesia and Intensive Care at Medical University of Vienna. nutritionDay Project Head
How can we utilize ESPEN NutritionDay data to advocate for better nutritional care throughout Europe?
NutritionDay is a one-day-a-year, cross-sectional audit of malnutrition in healthcare settings. The aim is to also include primary care (currently 2958 inclusions). Participation is free, easy, puts the patient first, gives feedback to the healthcare providers, has no language barrier, and provides a clear report. The next NutritionDay will take place on November 9th, 2023. Previously, 63 countries, 35 languages, and 15,000 units participated in this study.
Some results of the first cohort (2016-2019) are as follows: The Patient – And Nutrition – Derived Outcome Risk Assessment Score (Pandora) is a predictive score for 30-day in-hospital mortality based on demographic data, clinical observations, and nutrition. This shows, for example, that the day of admission is related to the outcomes for the patient, patients admitted on the weekend have a 50% higher chance of mortality. And that longer admission leads to a reduction in BMI, but a lower BMI also leads to longer admission. When patients are limited in their mobility, the mortality risk increases.
85% of hospital admissions are from the home situation, which means that nutrition prior to admission is also important. The less you eat, the higher your risk of death. However, patients often do not know what they are eating, and they eat much less during admission. This ‘missing data’ is important to face, and the cause must be found out.
It is therefore important to recognize that the characteristics of the patient are associated with outcome, risk profiles can prolong length of stay, risk factors are related, and no-eaters should always be acknowledged so that action can be taken. NutritionDay provides knowledge and awareness, benchmarking and a large reference database for further research.
Session 3: The future of continuity of nutritional care: how to set up for success?
Bianca Buurman
Chair of Nurses & Caregivers, the Netherlands & Professor of Acute Elderly Care Amsterdam UMC
Optimizing collaboration between primary care, hospitals, and care homes. Nurses connecting the dots.
After acute admission, the elderly are vulnerable, 15-20% are readmitted within 30 days, within 3 months after admission 20-30% experience functional limitations, and 20-30% die. This is why it is so important that everyone works together and that a better transition (hospital to primary care) of care is created.
Interventions start in the hospital and are continued at home, but research has shown that this has not yet resulted in an improvement in physical functioning, but slightly less mortality. The mechanism behind hospital-associated disability is not yet clear. It is clear that this is a multifactorial problem, such as age, limited mobility, geriatric problems, and limited social environment. But also, malnutrition and problems with food preparation. 51% of the elderly experience a loss of appetite on admission, 34% still experience this at discharge, and 28% one month after discharge. This is associated with lower muscle strength and mobility. Three months after discharge, 80% are below the cut-off value for muscle mass, 18% are limited in muscle strength, and 43% are in physical activity.
By optimizing the transition within the lines of care and across the breadth of care, readmission can be prevented, daily functioning is promoted, and this benefits the quality of life. We need to make better guidelines and train healthcare professionals. Collaboration between nurses, doctors and paramedical professionals is essential that does not stop with discharge but is continued post-discharge.
Maurizio Muscaritoli
Coordinator, Residency School in Internal Medicine presso Sapienza Università di Roma
From education to implementation: investment in the future.
The ESPEN working group ‘Nutritional Education in Medical Schools’ (NEMS) has described a minimum set of nutritional knowledge for medical students. Doctors must be able to recognize the importance of nutrition in terms of health, prevention, and treatment of disease. They must also understand the basic principles of human nutrition, understand nutrition-related issues, provide generic nutritional advice, and identify patients at risk of malnutrition so they know when to refer. A factsheet has been developed and a manifesto has been described. A toolbox is currently being developed for educators so that nutrition education can be easily implemented in the curriculum. This toolbox contains slides with the minimum required knowledge about basic nutrition, applied or healthy nutrition, and clinical nutrition. This includes information about micro- and macronutrients, metabolism, digestion and absorption, energy balance, body composition, nutritional guidelines, nutrition in life stages, prevention, and all types of medical nutrition. The aim is to present this toolbox at ESPEN 2023.
Gerda Pot
Program Coordinator, Nutrition and Health Scientist, Chrono-nutrition specialist, Lecturer
A Matter of Taste
You can taste good care! The aim is to optimize the nutritional environment for patients, staff and visitors in 50% of hospitals in the Netherlands by 2025. In 2030, all hospitals should have a healthy food environment. Other sectors in the healthcare sector are also involved.
Examples of improvements include offering whole-wheat bread as standard in hospitals and offering sugar-free drinks and water. In addition, only snacks that fit within a healthy diet are offered. 75% of Dutch hospitals are now connected to the initiative ‘You can taste good care!’. The program offers an online learning environment, masterclasses for chefs, a network for dieticians, toolkits on a website, clear communication and the provision of knowledge through collaboration with the research institute of Wageningen University.
Success-factors for implementation are an approved vision by commitment from the board and having a clear business case. Driving forces are dedicated nutrition assistants, coworkers as ambassadors and using storytelling and experiences.
An impression of the initiative can be viewed at:
Video URL: https://www.youtube.com/watch?v=UGW66-cY-zY
Summary ONCA day 2
Interactive break-out workshops: getting things done in Nutritional Care, round #1 and #2
Implementing GLIM: where are we and where are we going?
The GLIM criteria are well validated, many validity studies have been done. The advice for implementation is also not to wait for more validation. The criteria will be evaluated every 4-5 years. The measurement of muscle mass and inflammation was not yet sufficiently applied by the users. Guidance on how to measure muscle mass just has been published and by the end of this year a similar report will be published on how to measure inflammation.
The GLIM implementation working group has set up a survey in which barriers and opportunities have been asked for the implementation of the GLIM criteria. The biggest barriers were insufficient knowledge about the implementation process and priority within the organization. Dietitians felt the most involved but recognize that it is an interprofessional process. The use of existing screening methods was also seen as a barrier, but this can actually yield benefits when using the criteria. In addition, research in older patients during hospitalization has shown that the sensitivity and specificity of various screening instruments was low against the diagnosis based on the GLIM criteria, meaning we miss a lot of malnourished patients in the first step of the framework. Electronic patient files show potential for optimalization by implementing items of the GLIM criteria within the electronic patient files.
Advancing your local ONCA campaign: engaging decision-makers in your Malnutrition awareness week.
Three best practices were presented in this session.
In France, a Malnutrition Awareness week has been organized for the 4th time, 2.000 partners have now joined, more than 3.000 activities have been registered, which have led to 15.000 actions. Public funding has proved to be very important in this respect. The bottom-up approach is important, in other words, putting patients and healthcare providers side by side. It is also important to put the theme on the political agenda. In France, they have also publicized the subject through the postal service for the widest possible reach.
In the Czech Republic, the Ministry of Health is closely involved. They support the issuing of certificates and drawing up guidelines. In the meantime, 350 licenses of clinical nutrition have already been distributed. It is important to make the subject ‘sexy’, to give policy makers something that will enable them to become successful and to talk not about malnutrition but about ‘nutritional related disorders’.
In Germany, a Malnutrition Awareness week was organized for the first time. They have published a position paper and included screening and evidence-based nutrition in hospital policy. They have started creating an alliance, in which 25 societies are now affiliated, together accounting for approximately 120.000 doctors. As a result, politicians are also interested, and the discussion takes place in parliament. Politicians are invited to all activities.
The key to successful implementation of nutrition in education.
Through ESPEN’s ‘Nutritional Education in Medical Schools’ (NEMS) working group, a toolbox is being developed to embed nutrition in the medical curriculum. Challenges are the limited amount of time, the introduction of the topic and the limited opportunity for repetition. There also seems to be little attention for nutrition. Opportunities include involving students in the development of the toolbox and evaluation of the implementation, promotion through peer-to-peer invitations or even making nutrition education compulsory.
Prehabilitation can enhance recovery after surgery.
The ERAS protocol was discussed, and barriers to implementation were also discussed. The biggest obstacles were time, resistance in the field, and insufficient recognition of the problem. This, while it has been proven that it works. Among other things, the possibility of applying an audit was discussed, although this is difficult in healthcare. It is important to convey that the application may be more expensive than standard care but proves to be cost-effective. In addition, the window of opportunity to start with prehabilitation was discussed, which is not used in its optimum at the moment.
Health indicators: a multilevel approach to malnutrition coding.
Discussions are currently held with the ICD working group and the WHO. Soon the ICD-10 will be replaced by the ICD-11, ESPEN wants the diagnosis of malnutrition to be included in this. At the moment, only the code ‘underweight’ exists for people with a BMI below 18.5 kg/m2. It is a lengthy process to get all this done, while the proposal is widely endorsed.
Flavors of the World: supporting patients throughout Europe: a powerful awareness tool.
This workshop tried to put science on the plate. There has been spoken of compliance in nutritional care. The call was not to focus on nutrients in the conversation about nutrition, but on the question ‘Why do you eat’. By discussing emotion, the social function of food and taste, you create more conversation and promote compliance. To give an idea of what patients face cookies and chocolate were offered at the workshop, which turned out to be altered in taste.
Reporting of the ONCA pre-conference patients session.
The focus of the patient session was that they would rather look at possibilities and opportunities than at problems. All possible solutions must be put on the table so that the patient can see concretely what is feasible and can discuss the steps taken. There is a call for the patient association to be more active, to cooperate nationally but also across borders. An event will soon be organized (for example with stakeholders) in which nutrition is central but in which no food is offered, in order to bring the importance of nutrition to the attention of the guests even more.
Update on the Optimal Nutritional Care for All campaign.
The aim is to translate nutritional care and science into policy. By exerting influence within organizations and at policy level, they try to draw attention to the importance of optimal nutrition. But also, collaboration across different associations and fields is important to create influence on a European level.
ONCA is visible in Europe and various working groups have been formed, 20 countries have now joined, the last being Hungary. Cooperation with Norway is planned.
Meanwhile, 13 Malnutrition Awareness weeks have been organized, there are many ideas and inspiration that can be consulted via the ONCA website: Optimal Nutritional Care for All (european-nutrition.org).
Deep dive, the future of nutritional care
Peter Weijs
Professor Nutrition and Exercise at Amsterdam University of Applied Sciences
Protein transition: future world or fantasy land?
There are 3 major problems worldwide: obesity, malnutrition, and climate change. The latter also causes a health crisis, which may not yet be recognized. We can prevent the death of possibly 11.1 million people per year by adopting a plant-based diet. The plant-based diet also saves the environment through reduced CO2 emissions. However, this is complicated by increased water consumption. It is a complex system. The message, for now, is that red and processed meat should be limited and that we should eat more plant-based.
The EAT lancet has drawn up advice for a healthy and sustainable diet, for example, we should go from 60% animal and 40% vegetable food to a reverse situation. Therefore, it is not a complete vegan diet, which is a common misconception, as it still contains 84g of meat and 250g of dairy. For the transition, it is important that this becomes available, accessible and affordable. More information and education must also take place. The guidelines must be adjusted and ‘food marketing’ must take place. Finally, it is important to apply this in healthcare, dietary advice and interventions.
However, there are also challenges, for example with vulnerable patients. With the shift to plant-based nutrition, it may not be possible to achieve an optimal amino acid composition in the diet, so that protein synthesis is not sufficiently promoted. A plant-based diet also contains a higher fiber density and a lower energy density, which does not go well with the appetite of vulnerable patients, since the alternative diet comes with a higher volume to eat and has a faster saturation. The protein quality can also be discussed, for example, to replace 70 grams of meat, 1 kilogram of potatoes must be eaten. Of course, it is possible to make protein mixes, but this again belongs to the ultra-processed foods. All in all, it will mainly be about changing consumer behavior, which takes time.
Harriet Jager-Wittenaar
Professor of Malnutrition and Healthy Ageing, Hanze UAS
The future of nutritional care
Proactive, early and interprofessional treatment, that’s what we have to stand for. Much has now been developed in the field of screening and the accessibility of medical nutrition. The GLIM criteria are also a success. However, intervention is often too late despite the use of screening. Not all screening tools cover the GLIM criteria and each tool measures different facets of malnutrition. This creates a difference in the recognition of patients at risk. Research shows that the choice of screening instrument used in healthcare has an effect on the length of stay.
We must therefore reconsider the ‘risk of malnutrition’ and, above all, record how we identify this risk. There are 6 key factors for the interprofessional treatment of malnutrition, that is shared commitment, shared identity, clear goals, clear team roles and responsibilities, interdependence between team members and integration between work and practice. Research has been done into this collaboration construction, which shows that professionals are positive and want to work together, but that the interprofessional identity in particular between the professions is still significantly different.
Lorenzo Donini
Full Professor of Food Science and Human Nutrition at Sapienza University of Rome
The collision of two epidemics: sarcopenic obesity.
Among the over-60s, 10-37% have sarcopenia, estimated to cost $397 million by 2028. Sarcopenic obesity is a clinical and functional condition characterized by obesity, high fat mass and sarcopenia, or low muscle mass and function. The awareness of sarcopenic obesity is completely absent. Sarcopenic obesity creates a pro-inflammatory milieu which in itself has an adverse effect upon skeletal muscle. Other potential mechanisms behind sarcopenic obesity are physical inactivity, selective undernutrition (energy dense nutrient-poor diets), impaired motor neurons and obesity-related chronic conditions. In older adults, sarcopenic obesity is associated with decreased functional capacity, poor nutritional status and a higher level of cognitive decline. It could be seen as a switch from absolute sarcopenia to relative sarcopenia. For example, although an obese person with sarcopenia is still very physical active, they still are in a pro-inflammatory state and have fat infiltration within the muscle, the quantity of the muscle might stay the same but the quality of the muscle decreases.
ESPEN and the European Association for the Study of Obesity have jointly written a consensus statement discussing screening, diagnosis and staging of this syndrome. The Sarcopenic Obesity Global Leadership Initiative (SOGLI) will have their next meeting in November 2023.
See also: Donini LM, Busetto L, Bischoff SC, Cederholm T, Ballesteros-Pomar MD, Batsis JA, Bauer JM, Boirie Y, Cruz-Jentoft AJ, Dicker D, Frara S, Frühbeck G, Genton L, Gepner Y, Giustina A, Gonzalez MC, Han HS, Heymsfield SB, Higashiguchi T, Laviano A, Lenzi A, Nyulasi I, Parrinello E, Poggiogalle E, Prado CM, Salvador J, Rolland Y, Santini F, Serlie MJ, Shi H, Sieber CC, Siervo M, Vettor R, Villareal DT, Volkert D, Yu J, Zamboni M, Barazzoni R. Definition and Diagnostic Criteria for Sarcopenic Obesity: ESPEN and EASO Consensus Statement. Obes Facts. 2022;15(3):321-335.