
The Optimal Nutritional Care for All Conference 2018
18 Countries, One Mission - Sintra, Portugal, 12 & 13 November 2018
18 Countries, One Mission - Sintra, Portugal, 12 & 13 November 2018
Conference poster
Delegations from each member country including industry representatives joined colleagues for two days of presentations, workshops and discussions on topics ranging from influencing public policy, collaborative research and driving patient-centred care in every setting.
The 2018 Conference took place 12th-13th November in Sintra, Portugal. The campaign is grateful for the support offered by the Portuguese delegation, the Mayor of Sintra’s office and the Portuguese Ministry of Health.

The 5th annual Optimal Nutritional Care for All conference in Sintra, Portugal was opened by Anne de Looy, who welcomed delegates and Portuguese attendees of the opening ceremony. She described the vision of the campaign to create a world where every patient who is undernourished or prone to malnutrition is screened. Malnutrition is everyone’s business. The Optimal Nutritional Care for All campaign builds on and accelerates best practices. We have become very much a family of professionals coming together. Let’s be the generation that turns the vision into a reality.
Olle Ljungqvist, Co-chair ENHA
In his presentation “Why the Optimal Nutritional Care campaign?”, Olle Ljungqvist highlighted the unique position of the campaign due to its great reach across 18 European member countries. Beyond its role as an international campaign, driven by policymakers and professional organisations, the campaign moreover provided the necessary depth by bridging the often-experienced gap between patients and healthcare providers, he argued, thus bringing all stakeholders across the nutritional care pathway together. Shared decision-making and meaningful patient involvement were key in improving nutritional care treatment and outcomes, he stated.
Ljungqvist argued that more access to nutritional care was needed across the patient base, as malnutrition formed a very important part of acute and chronic disease. Malnutrition and its consequences are highly costly for health systems across the European area. In order to effect lasting change, there was a need for data-driven research, he argued. Olle Ljungqvist reported on the ERAS project (Enhanced Results After Surgery) and highlighted the importance of training and audit in effective nutritional care provision and improvement.

Katie Gallagher, European Patients Federation (EPF)
Next, the audience heard from Katie Gallagher from the European Patients Forum (EPF) who pledged that it was a public policy priority to raise health literacy and awareness of the role of nutrition in the management of long-term conditions among patients and decisionmakers. In order to achieve this, Katie argued, it was vital to coordinate the patient perspective to meaningfully involve them in the process.
To this purpose, EPF are launching a paper in collaboration with ESPEN which provides lay versions of patient guidelines in accessible format to facilitate stronger patient involvement in nutritional care. In the creation of these guidelines, a great focus has been on patient input, in order to make the guidelines as accessible and adapted to the patients’ needs as possible. [Download presentation]

Portuguese MEP Sofia Ribeiro
Discussing the value of nutritional care for European citizens and EU support, Portuguese MEP Sofia Ribeiro underlined the role of the EU as a social actor, outlining the contributions the EU has made to nutritional care provision. Sofia Ribeiro argued that the EU was instrumental in aiding EU member states to achieve shared objectives in nutritional care and prevention standards. Moreover, the EU’s “from farm to fork” food safety policy provides a guaranteed baseline of nutritional standards throughout the European region. She highlighted the EU-wide School Fruit, Vegetable and Milk schemes to encourage healthier eating from a young age, as well as the New Alliance for Food Security and Nutrition, which seeks to introduce higher nutritional standards on an international level.

José Inácio Faria, Portuguese MEP
José Inácio Faria, Portuguese MEP and member of the EPP group on environment, public health and food safety, highlighted that effective nutritional care was paramount given the increase in comorbidities resulting from ageing population trends. In order to enhance physical activity, diets and health across the life course, the EU has implemented regulation to make nutritional information available on all packaging, whilst limiting the advertisement of unhealthy foods. While progress has been made, Faria argued that stricter measures needed to be in place to ensure better health outcomes.

Basílio Horta, mayor of the city of Sintra
Following the keynote addresses, Basílio Horta, mayor of the city of Sintra welcomed delegates to the conference. “The health and wellbeing of our citizens is the priority for Sintra government. We are looking to increase accessibility to healthcare – both primary and secondary, as well as ensuring better commitment to labelling in the food industry.”
To this end, the mayor reported that the local government had negotiated for the construction of five new healthcare centres and a hospital, as well as for the development of a plenary health plan with the Ministry of Health. Basílio Horta welcomed the cooperation with the Optimal Nutritional Care for All campaign and APNEP (Portugese PEN Society) and was looking forward to the high-quality content of the conference to promote international cooperation in the campaign for optimal nutritional care for all.

Aníbal Marinho, president of APNEP
Next, the audience welcomed by Aníbal Marinho, president of APNEP and chair of the Portuguese organising committee, who reported on the work of APNEP, one of the largest healthcare societies in Portugal with more than 2,000 conference participants each year. Aníbal thanked the Optimal Nutritional Care for All campaign for helping the organisation receive government backing for outpatient support and support of patient associations on a national level. He added that APNEP had been able to take advantage of the 2018 conference to optimise nutritional support for the local population by enabling nutritional screening, for adults and paediatrics, in all public hospitals.

Céu Machado, Infarmed
Discussing nutritional care outcomes in Portugal, Céu Machado from the government health agency Infarmed discussed that despite growing awareness campaigns, obesity remained to be on the increase, “threatening a medical emergency”. Rates of obesity of 20- to 40-year-olds had doubled between 1992 and 2002, she stated.
OECD data revealed that family spending on fruit and vegetables had significantly decreased during the last financial crisis. Malnutrition presents a real challenge, Machado argued, one which government should make a policy priority. “Health is the basis to the capacity to handle the physical and emotional challenges throughout everyday life”.

Paula Castelões, Royal College of Physicians
Paula Castelões, Royal College of Physicians, argued that “malnutrition is a current and pertinent matter for public health”. In order to alleviate the problems associated with malnutrition, she pledged for the creation of more working groups to ensure quality care for patients.

António Sales, member of the Portuguese Parliament
Finally, António Sales, member of the Portuguese Parliament, argued for the importance of an integrated care model in Portugal.
“Today we live in a free, open Europe – a Europe which can be proud of its cultural diversity, its commitment to defining citizens’ rights and common values.”
“If the EU wants to be a project that is fully alive again, it needs to demonstrate its ability to solve problems that are important to its citizens.”
Due to its links to increases in morbidity and hospital stays, policymakers needed to act on undernutrition and malnutrition imminently, argued António Sales. Nutritional screening (both parenteral and enteral) should be available in every hospital, he concluded.

Olle Ljungqvist
Following the lunch break, Olle Ljungqvist reflected on the high quality of speakers during the morning session. He expressed his delight at the fact that politicians and decisionmakers at all levels were sharing the same message, reflecting the goal of the Optimal Nutritional Care for All campaign to appeal to people across the care pathway to align their work to fulfil the vision of the campaign.
Jorge Falcato, European Health Committee
Jorge Falcato, on the European Health Committee started off the next session, in which he discussed the presence of growing inequalities in the Portuguese healthcare system. “Almost 2 million treatments didn’t occur in the last year due to people’s inability to cover healthcare fees.”
He argued that more needed to be done to combat the unequal health outcomes resulting from wealth discrepancies and malnutrition.
Ricardo Marinho
Ricardo Marinho further reported on the prevalence of malnutrition in Portugal. He presented his research findings from the Portuguese ANUMEDI study which revealed that 56% of patients were in moderate or suspected malnutrition with 17% severely malnourished. As such,
The research moreover strongly correlated malnutrition with illiteracy and recent hospital admissions. As such, he argued that socioeconomic factors were strong determinants of malnutrition, which were further exacerbated as a result of poor nutritional care.

Marek Lichota
Marek Lichota, representing the Polish patient organisation, discussed the importance of empowered patient involvement in nutritional care. He highlighted that the nutrition team not only consisted of physicians, nurses, dieticians and pharmacists but also the patient – a component far too often overlooked.
To not only enhance the patient experience, but to contribute to the optimisation of care. In order to facilitate patient empowerment, the provision of the right information at the right time, health literacy, digital literacy and mutual respect to facilitate shared decision-making, were key.
He presented his initiative, “Appetite for Life” as an example of meaningful patient engagement and empowerment to showcase the benefits of an inclusive approach. [Download presentation]

Harriët Jager-Wittenaar, EFAD
Next, delegates heard from Harriët Jager-Wittenaar, representing EFAD, who presented on good practices for effective nutritional screening and early malnutrition diagnosis. She argued that tackling malnutrition needed to be an interdisciplinary effort. Moreover, screening should not be the end goal, but rather the first step in the nutritional care process within a consistent feedback loop of evaluation. She also argued that in order to provide accessibility for all, malnutrition screening and assessment required validated, translated and cross-culturally adapted instruments. Screening and nutrition care should not only occur within the hospital setting. “The real window of opportunity for meaningful change is in the outpatient setting – before and after hospital admission”, she argued. [Download presentation]
António Sousa Guerreiro
António Sousa Guerreiro pledged for the inclusion of clinical nutrition education in the curriculum of medical schools to allow for the greater integration of healthcare and nutritional care provision. He argued that
and that more should be done to overcome barriers to this.

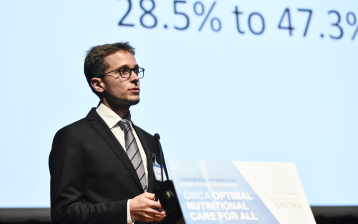
Joost Wesseling, Optimal Nutritional Care for All campaign
Finally, Joost Wesseling, Campaign & Operations of the Optimal Nutritional Care for All campaign, presented on how to “build an audience”. He showcased the growth of the campaign and underlined the importance of spreading the campaign, not merely by discussing research findings within the campaign’s community but by making nutritional professionals, policymakers and members of the public aware of the importance of optimal nutritional care for all. He conducted an interactive micro-workshop to show delegates how easy it is to share a Good Practice with your peers. He appealed to delegates to make better use of these resources to allow the campaign to grow.

In the first breakout session, Annemarie Perl and Cornel Sieber presented on findings from the SHARE database (survey of health, ageing and retirement in Europe). Annemarie described how her team had cleaned the data and used the last three waves of the longitudinal study to show that across Europe, there was a great correlation between advanced age and malnutrition. People above the age of 70 were 4 times as likely to be malnourished or at risk of malnutrition than their younger counterparts. Her analysis served as an example for a discussion on which factors from the data could be combined to draw interesting conclusions on nutritional care outcomes across Europe. Breakout participants discussed relevant data clusters from the survey points that could be drawn together and built upon. A number of countries put down their details to look into collaborating on projects using the cleaned SHARE data. Country delegations’ progress will be shared via the website and in upcoming conferences.

The second breakout session was led by Katie Gallagher from EPF with speakers including Cristina Cuerda, Carolyn Wheatley and Isabelle Manneh who discussed initiatives and pathways for patient involvement in nutrition care. Katie Gallagher reported on the creation of the EPF/ ESPEN patient guidelines and the importance of continual patient involvement in the process of this. Cristina Cuerda from ESPEN moreover added that the lay versions of patient guidelines to be published by ESPEN would be translated into national languages in order to remove linguistic and cultural barriers to access the information. She discussed ESPEN’s aims to disseminate these broadly, such as through apps and other dissemination channels.[Download presentation] Carolyn Wheatley presented on BAPEN’s campaign on increased patient involvement, as well as the creation and dissemination of guidelines and leaflets to help put the patient at the centre of nutritional care. [Download presentation] And finally, Isabelle Manneh added her perspective from ECPC. As a recognised voice for cancer patients, following patient consultations, ECPC has published a number of booklets and guides from patients for patients to increase accessibility of information for the empowered patient. [Download presentation]

In this break-out session, Rudi Crabbé (Eten & Welzijn Foundation) and Marcel Smeets (ENHA Trustee) analysed success factors for national ONCA campaigns. On the basis of the Dutch “Green deal” (a bottom-up inter-sectoral alliance of stakeholders and government) and the French (top-down government-initiated) campaign “La maison gourmande et responsible”, they identified several common characteristics which should underlie a successful campaign. Firstly, the campaign should be based on a basic idea to frame the initiative. There needs to be a clear and identifiable initiator to build a national alliance and kick-start the campaign. A campaign should set clear objectives under a sound and comprehensive message. And finally, it requires credibility and support to gain as much traction as possible.
The following discussion focused much on the key role of credibility and how it may be achieved. Delegates argued that patient engagement from the start was key in orienting actions and in providing necessary credibility for messaging and goals.
The break-out session concluded with three take-away messages for future campaigning, namely the development of a modular campaign template that could be adapted across the campaign’s region to national needs. Secondly, participants argued that the Optimal Nutritional Care for All campaign could greatly benefit from “influential communication” training by professional communication strategists. Regular updates and sharing of good practices via the ONCA website and meetings should be further encouraged and supported by all national delegations. [Download presentation]

Following the breakout sessions, all delegates returned to the hotel before departing for the conference dinner at the National Palace of Sintra, kindly hosted by the City of Sintra. Delegates received a tour of the palace, followed by a networking reception. Frank de Man, Executive Director of ENHA took the occasion to thank the council of Sintra and the Portuguese hosts for their dedication and hospitality.
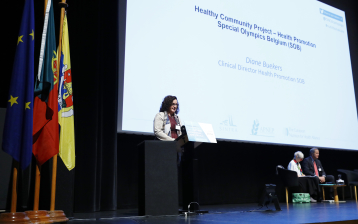
Diane Buekers
Starting off the session on innovation, delegates heard from Diane Buekers, who presented a case study of the Belgian Special Olympics for people with intellectual disabilities. Many people with intellectual disabilities have problems with particular types of food and as a result, a great proportion is malnourished.
She reported on the Healthy Athletes Programme which offered free health screenings and nutritional education as part of the sporting events. Moreover, the initiative offers the Healthy Community Project, year-round programmes to help people with intellectual disabilities. Under the theme of “food as a festivity”, the Belgian HCP has organised 6 events so far in care homes which involved fun activities for patients, alongside the serving of personalised adapted food. Diane showed a video of the project’s first event and said that the initiative had gained a great deal of media and public attention, engaging the Secretary of State for People with Disabilities, the Ministry of Health and a great number of Belgian health organisations. Having curated a recipe and a sports booklet for participants, HCP has plans to become a sustainable project. [Download presentation]

Ronit Endevelt, Israeli Ministry of Health
Next, Ronit Endevelt from the Israeli Ministry of Health presented on the benefits of oral and physical assessment as a tool for improving nutritional treatment. She argued that malnutrition and dental status of an individual were closely interrelated, as causes including low socioeconomic status, functional limitation, chronic disease or cognitive impairment may lead to poor oral hygiene or an inability to take care of one’s teeth. As a result, the loss of teeth, pain or biting difficulties could impair an individual’s ability to eat healthy foods such as fruit and vegetables, thus leading to poorer nutrition. She argued that oral health screening should be included in nutrition screening. The Israeli Ministry for Health has provided training to dieticians, especially in care homes, and the intervention has improved patient care outcomes. As such, Ronit Endevelt pledged for a physical assessment of head, neck and oral health as part of nutritional assessment to better inform personalised nutrition plans to facilitate improved nutritional care and quality of life. [Download presentation]
Gaston Remmers
Gaston Remmers concluded the session on innovation with a presentation on patient-driven research in nutrition. He identified a feedback vacuum in the nutritional care pathway and innovation. Mr Remmers argued for a need to operationalise everyday food practice to allow the everyday experience of patients to upcycle to food sciences and create an active feedback loop.
To illustrate his point, he introduced the example of the Food Basket for Prostate Cancer, a trial study of 250 men suffering from prostate cancer. Within the trial, participants had short and easy-to-complete assessments 4-5 times a day, alongside on-the-spot personalised questions. This not only allowed patients to receive immediate feedback on their nutritional status and receive tailored and personalised care, but moreover provided an ideal opportunity for therapists and researchers to follow their patients and receive insights into the effectiveness of their approach. Patient involvement was not only key in improving treatment outcomes, but moreover had the potential of informing research, he argued. [Download presentation]

After an introduction round, this breakout session, chaired by Gaston Remmers and co-chaired by Katie Gallagher, started off with a thirty-second introspection on what the most pressing issues were for patient delegates. The main conclusion was that there is an opportunity to further improve the patient focus of the conference. This could be achieved by not only asking patients for feedback, but by actively including patient representatives in the campaign’s programme development. Suggestions included inviting local patient organisations to ONCA workshops and conferences with a concrete theme to encourage engagement, setting up more regular meetings (potentially via Skype), making the logistics and schedule of events more compatible with the needs of patients and making patient involvement and empowerment a standard component of every speaker’s presentation.
Further remarks included the encouragement of an EU-level coordinated patient network and the promotion of sharing good practices throughout the year.


The industry session determined four key drivers for the upcoming year. Firstly, industry representatives argued for the creation of a stronger and more specialised evidence base to be used across the health care community. Moreover, they agreed that more should be done to share local Optimal Nutritional Care for All campaign good practices and benchmarks through virtual platforms, as a means of spreading the campaign beyond the realms of the campaign’s community. And finally, delegates pointed out that malnutrition needed to be made accessible and attractive to policymakers in order to achieve change.
Rocco Barazzoti, Chair of ESPEN
Following the morning breakouts, delegates returned to the main auditorium for the final afternoon session, which was started by Rocco Barazzoti, Chair of ESPEN. In his speech, he presented the Global Leadership Initiative in Malnutrition (GLIM) assessment criteria of malnutrition, which could serve as a set of simple consensus criteria intended for global application and requiring only moderate training. GLIM is based on readily available assessment tools and methods, making it widely applicable and allowing for the easier spread and harmonisation of nutritional screening internationally. He argued that it would be possible to combine the GLIM method with further approaches and criteria based on regional preference to make it more exact and better-suited to the context to which it is being applied.

Prof Dr. Meltem Halil
Prof Dr. Meltem Halil presented on the IAMAP project in Turkey which is seeking to support a more bottom-up approach in nutritional care. Currently, nutritional care and awareness is only present in secondary and tertiary care in Turkey, meaning that many people affected by or at risk of malnutrition are not receiving adequate care. The project team are planning to provide nutritional training to primary healthcare professionals and integrate nutritional screening tools in primary healthcare policy over the course of the next three years. Launching in January 2019, the project team will report back to the Optimal Nutritional Care for All campaign on the progress of the initiative.
Next, participants of the morning breakout discussions reported on the key recommendations to take ahead for the next year of the Optimal Nutritional Care for All campaign and to serve as a basis for the forward planning of the campaign in upcoming years.

Patrick Kamphuis, MNI representative

Frank de Man, Executive Director of ENHA
Following the reports from delegates, Frank de Man, Executive Director of ENHA, contributed his view for the future of the campaign. Due to the interdisciplinary and ever-changing field that the Optimal Nutritional Care for All campaign was addressing, Mr De Man argued that the campaign needed to adapt over the years. He welcomed delegates to send in their comments and ideas. The main objective for the campaign moving forwards should be to create impact, he argued. This should occur through the broadening of the internet campaign under participation of all members to push for the inclusion of nutrition in healthcare education and practice, as well as deliver practical opportunities for countries to grow. He thanked all delegates and the organising committee.

Chair Anne de Looy
Finally, chair Anne de Looy shared some closing remarks with the conference attendees. She highlighted the great engagement of MEPs and MPs with nutrition over the last two days. Now the next step needed to be implementation and putting ideas into practice, she urged. In order to achieve this, it was necessary to work together – patients, industry and governments – to bring the message out there. She underlined the value of a coordinated communications strategy, with particular attention to the role of the website as a platform for knowledge exchange to allow the campaign to continue to grow.